Description
Course type: Online; Self-Paced
Specialty: Specialty: Cardiology
Language: English, Portuguese
Resources: Debriefing Videos
Level: Intermediate / Advanced
Target: Medical doctors
Modules: 16
Durations: 2 months
Time Effort: Up to 110 minutes per module
Certificate: Yes
Course Description
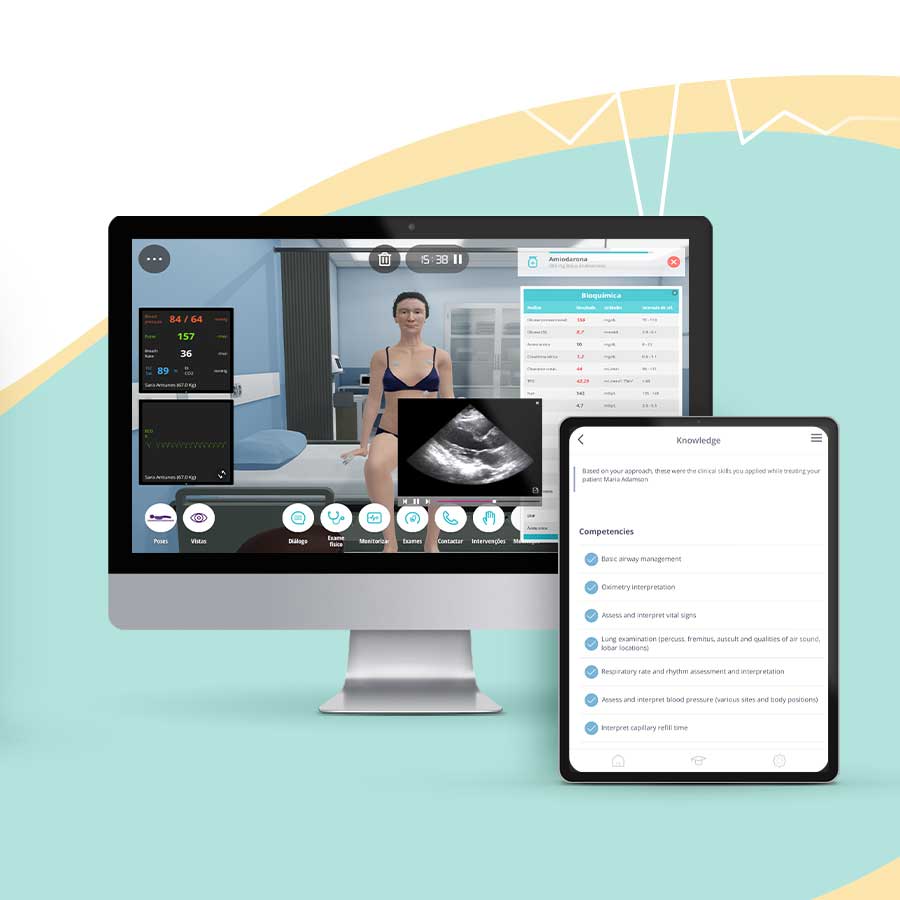
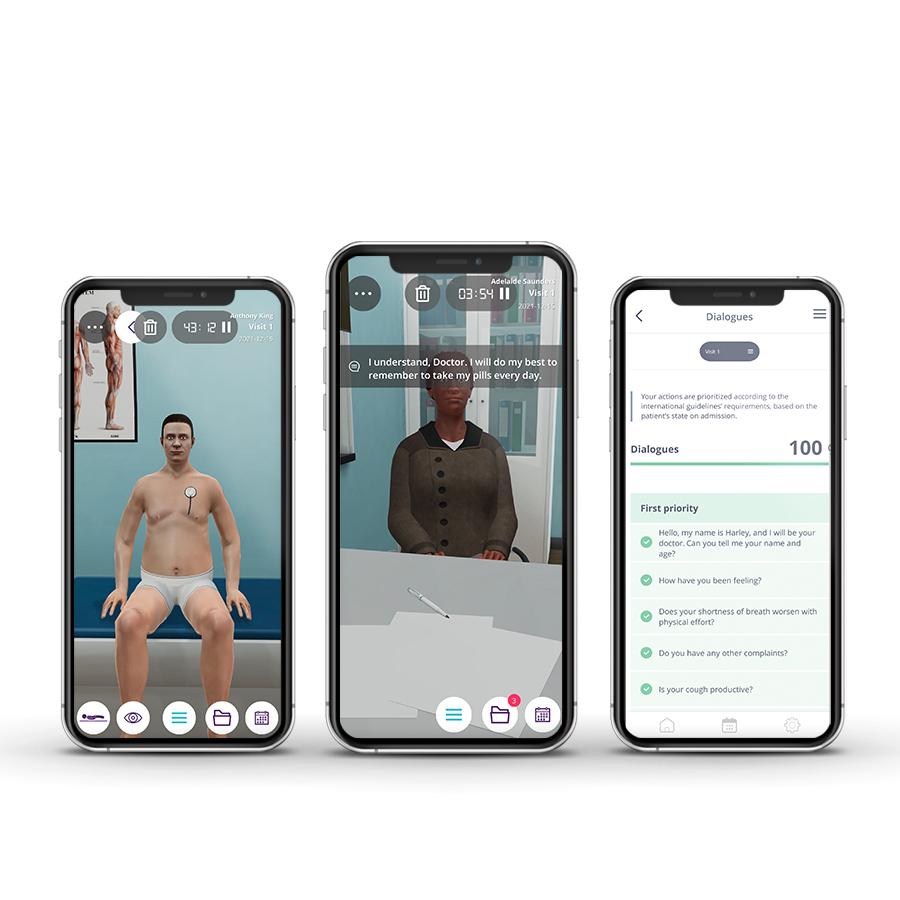
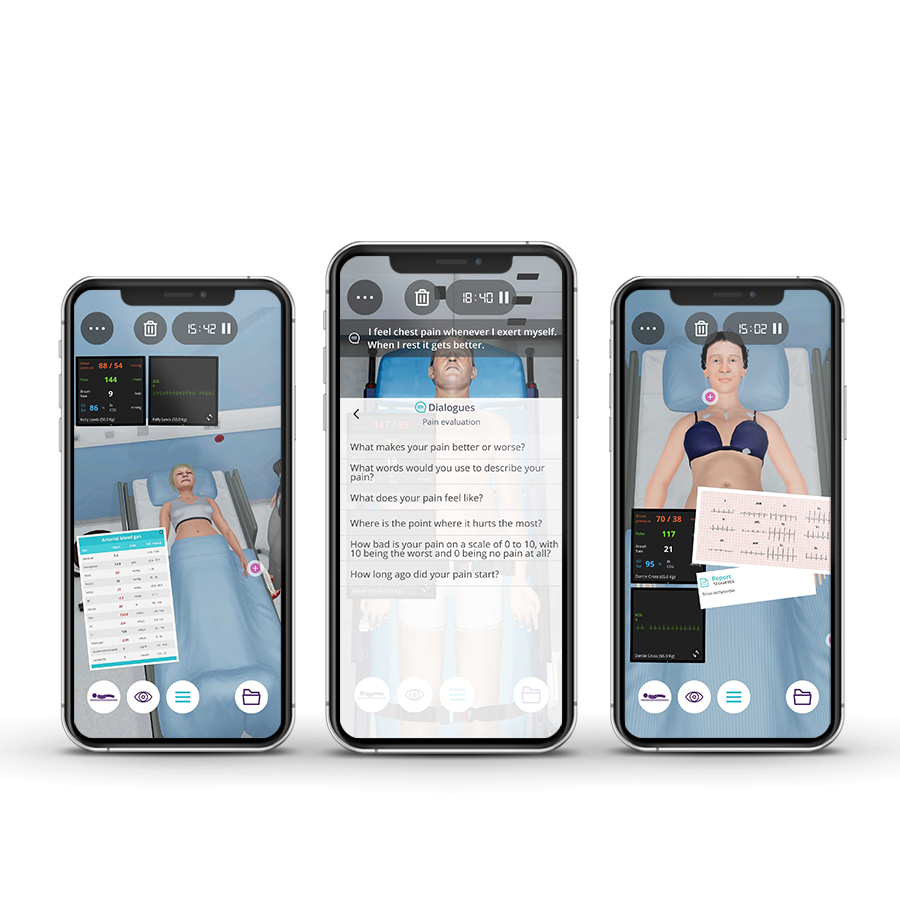
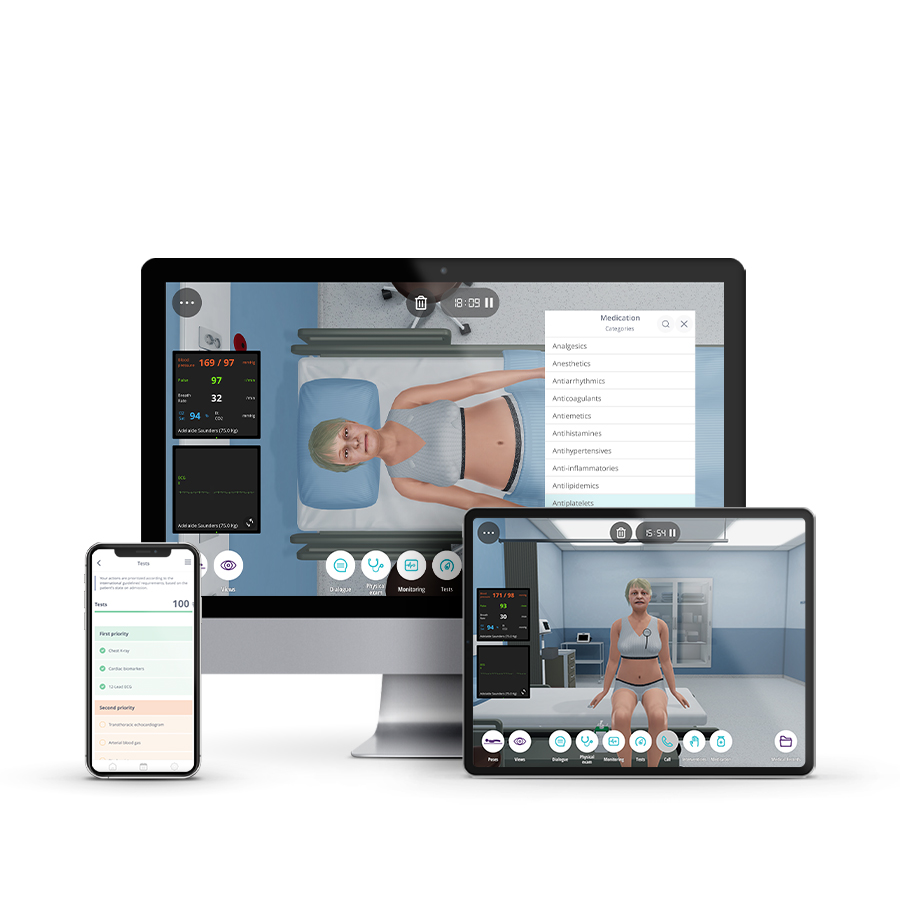
Virtual Patients are now a complementary tool in clinical training and support healthcare professionals, to apply their knowledge into practice and to actively learn through this immersive technology experience.
The Online Masterclass in Cardiovascular Emergencies, is designed for pre and post-graduate Students and Medical Professionals, to enhance their clinical reasoning and decision-making skills. This course also trains participants in the correct procedures for patient stabilisation and to manage any underlying disease.
Course Overview
- 16 Modules
• 16 virtual patient cases of an intermediate level of complexity - 3 Webinars
• With medical experts from the Lisbon School of Medicine - Average Time to practice (per module):
• Clinical Scenario: 20 minutes per attempt (3 attempts: 60 minutes)
• Final attempt (if applicable): 20 minutes
• Multiple Choice Question: 5 minutes
• Feedback Area: 10 minutes
• Learning Objectives and Scientific References: 10 minutes
• Debriefing Video: 10 minutes - Online, Self-paced
• You have up to 2 months to complete the 16 modules at your own pace. The course can be accessed through Body Interact at any time. - Certificate of Completion
• Certified by Lisbon School of Medicine - 2 ECTS
Learning Objectives
• Perform the correct procedures for the patient’s stabilization and manage any underlying disease
• Perform Echocardiography to identify tamponade
• Learn how echo helps to exclude mechanical complications (acute MR, ventricle septum or free wall rupture) after acute MI
• Learn how echo reveals systolic and diastolic function of the LV and gives important information on filling pressures
• Learn how echo gives information in the right ventricular function which is particularly important considering assist device implantation
• Learn how echo can exclude pericardial effusion as a cause of cardiogenic shock
• Learn how echo visualizes Thrombi
• Search for indirect signs of constriction in echo
• Call Cath Lab to perform pericardiocentesis
• Identify ventricular tachycardia using electrocardiography
• Correct heart rate to normal by administering IV medications or electrical therapy
• Learn how echocardiography represents a fundamental diagnostic tool for patients presenting to the ICU for dyspnea
• Identify life-threatening conditions, such as complicated infective endocarditis (IE), requiring immediate treatment
• Identify large, mobile vegetations, left ventricular systolic dysfunction and severe aortic regurgitation
• Understand the right heart failure physiology and the optimised way of treatment
• Focus on specific clinical manifestation of pericardial diseases
• Understand the role of early echocardiography in patients admitted to ICU due to decompensated heart failure
• Evaluate diastolic function in patients with pericardial diseases
• Properly treat Gastrointestinal haemorrhage and control the blood loss
• Perform coagulation tests to assess the patient’s coagulation status and discuss anticoagulation reversal
Module 1 – A 68 year-old man with dyspnea and fever
Virtual Scenario: Wilson was dining with his wife at home. Suddenly he felt breathless and weak and was brought by his wife to the Hospital.
Module 2 – A 60 year-old man with recurrent dyspnea and abdominal distension
Virtual Scenario: Sally was in her garden, doing some gardening, when suddenly she felt her heart racing as well as chest discomfort. She called the emergency unit as soon as she could and was brought to the Hospital.
Module 3 – Beyond cardiac pathology
Virtual Scenario: Kenneth had just recently fought a terrible flu and, due to his frail health, stayed mostly at home. Suddenly he woke up during the night feeling terrible and his wife insisted that he needed an ambulance.
Module 4 – Sudden feeling of malaise
Virtual Scenario: Patient presenting to the emergency department (ED) for worsening dyspnea since 3 weeks ago; dyspnea at rest (NYHA IV) and orthopnea at presentation. Given the evidence of lung congestion at chest X-ray, the patient is admitted to the ICU.
Module 5 – Woman wakes up at night with chest pain
Virtual Scenario: Patient was referred to hospital due to persistent cardiogenic shock. With positive inotropic treatment, Levosimendan and negative balance, patient was stabilized. HF treatment was started and patient was referred to intermediate care. Despite treatment, patient did not improve and evaluation for VADs implantation and TPL was started. However, patient deteriorated and was referred to the ICU again.
Module 6 – Male felt persistent chest discomfort following a family argument
Clinical Scenario: Mickey suffered an aortic aneurysm rupture and was transferred immediately to a specialist heart and lung centre, for an emergency surgical repair of his ruptured aneurysm. Although Mickey was hemodynamically stable after surgery, 8 hours post repair his clinical condition severely deteriorated. He has suffered 2 strokes previously; the first was 2 and a half years ago and the second was 6 months ago.
Module 7 – Severe calf pain
Virtual Scenario: Mr Hayden’s health has deteriorated progressively during the past 5 years, significantly impacting his quality of life. During this period, Mr Hayden has been hospitalized several times, and has ended up hospitalized much more frequently in the past year.
Module 8 – Severe calf pain
Virtual Scenario: While going about her daily routine, Catherine felt ill: she vomited and noticed blood in her stool. Catherine then decided to go to the hospital.
Module 9 – Chest discomfort and palpitations
Virtual Scenario: While he was on a morning walk with his dog, Neal felt that something was wrong. Thankfully, a neighbour saw him and called for assistance.
Module 10 – Child with palpitations
Virtual Scenario: Stuart was having breakfast with his family. Following a brief argument with his wife, he started to feel persistent chest discomfort. He was immediately brought to the emergency department.
Module 11 – Symptoms and signs, never depreciate
Virtual Scenario: Adelaide was abruptly awoken during the night with crushing, substernal chest pain, and immediately sought medical care.
Module 12 – Acute dyspnea: Don’t Just Look, act
Virtual Scenario: One month ago, Kelly was hospitalized for chest pain and was diagnosed with acute myocarditis. Today she felt ill again and, once more, sought emergency medical care.
Module 13 – Relapsing heart disease
Virtual Scenario: Josh has been experiencing fever, and tummy and chest pain. The symptoms started 3 days ago.
Module 14 – Febrile syndrome with alarm signs
Virtual Scenario: Scenario context: Alexandra suddenly felt unwell when she was getting ready to go to school. Her mother noticed, and rushed her daughter to the Pediatric Emergency Unit.
Module 15 – Sudden dyspnea at night
Virtual Scenario: The patient has a history of intermittent claudication due to peripheral artery disease (PAD) in addition to multiple cardiovascular risk factors. He has been followed by his primary care provider over the past few months but for the past week the pain has worsened. A duplex scan of his right lower extremity shows stenosis. He is admitted to the hospital for further evaluation and treatment.
Module 16 – Sudden deterioration in a patient with a history of heart disease
Virtual Scenario: After having a discussion with his mother, Paul suddenly felt worsening of the chest pain he had been feeling. He immediately called the emergency unit and was brought to the hospital.
Authors and Speakers
With a multidisciplinary group of international clinical reviewers, Body Interact ensures a high standard of accuracy, diversity, and impact of its course.
Course Coordinator
Fausto J. Pinto
MD, PhD
Ana G. Almeida
MD
Speakers
Catarina Sousa, MD / Daniel Caldeira, MD / Gustavo Silva, MD / João Agostinho, MD / Miguel Menezes, MD / Tatiana Oliveira, MD
Scientific References
- Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS Guideline for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2017.
- Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Journal of the American College of Cardiology. 2021;78(22):e187-e285.
- Priori SG, Blomström-Lundqvist C, Mazzanti A, et al. 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC)Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). European Heart Journal. 2015;36(41):2793-2867.
- Braunwald E. Essential Atlas of Heart Diseases. 3rd ed. Philadelphia, PA: Current Medicine; 2005.
- Kasper DL, Fauci AS, Hauser SL, Longo DL, Jameson JL, Loscalzo J. Harrison’s Principles of Internal Medicine. 19th ed. New York: McGraw-Hill Education/Medical; 2015.
- Gerhard-Herman MD, Gornik HL, Barrett C, et al. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2016.
- Skellett S, Hampshire S, Bingham R, Maconochie I, Mitchell S. European Paediatric Advanced Life Support. London: Resuscitation Council (UK); 2016.
- Demmler GJ. Infectious Pericarditis in Children. The Pediatric Infectious Disease Journal.2006;25(2):165.
- Durani Y, Giordano K, Goudie BW. Myocarditis and pericarditis in children. Pediatr Clin North Am. 2010;57(6):1281-1303.
- Imazio M, Gaita F, LeWinter M. Evaluation and Treatment of Pericarditis: A Systematic Review. JAMA. 2015;314(14):1498-1506.
- National Institute for Health and Care Excellence (NICE) (2022). What are the signs and symptoms of cardiac causes of chest pain?
- Park MK. Park’s Pediatric Cardiology for Practitioners. 6th ed. Philadelphia, PA: Elsevier Saunders; 2014.”
- Hartman ME, Cheifetz IM. Pediatric Emergencies and Resuscitation. In: Kliegman RM, Stanton BF, St Geme JW, Schor NF, eds. Nelson Textbook of Pediatrics. 20th ed. Philadelphia, PA: Elsevier; 2016: Chapter 67.
- Horeczko T, Inaba AS. Cardiac Disorders. In: Walls RM, Hockberger RS, Gausche-Hill M, eds. Rosen’s Emergency Medicine: Concepts and Clinical Practice. 9th ed. Philadelphia, PA: Elsevier; 2018: Chapter 170.
- Skellett S, Hampshire S, Bingham R, Maconochie I, Mitchell S. European Paediatric Advanced Life Support. London: Resuscitation Council (UK); 2016.”
- January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation. Circulation. December 2014.
- 17. Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37(38):2893-2962.
- You JJ, Singer DE, Howard PA, et al. Antithrombotic therapy for atrial fibrillation: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e531S-75S.
- Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus Warfarin in Patients with Atrial Fibrillation. New England Journal of Medicine.2009;361(12):1139-1151
- Ewy GA. The optimal technique for electrical cardioversion of atrial fibrillation. Clinical Cardiology. 1994;17(2):79–84.
- Freeman JV, Zhu RP, Owens DK, et al. Cost-Effectiveness of Dabigatran Compared With Warfarin for Stroke Prevention in Atrial Fibrillation. Annals of Internal Medicine.2011;154(1):1-11.
- Furie KL, Goldstein LB, Albers GW, et al. Oral Antithrombotic Agents for the Prevention of Stroke in Nonvalvular Atrial Fibrillation A Science Advisory for Healthcare Professionals From the American Heart Association/American Stroke Association.Stroke. 2012;43(12):3442-3453.
- Haas CE. Monitoring Anticoagulation Therapy in the Critically Ill. Society of Critical Care Medicine. 2008.
- Hirsh J, Anand SS, Halperin JL, Fuster V. Guide to anticoagulant therapy: heparin: a statement for healthcare professionals from the American Heart Association. Circulation. 2001;103(24):2994–3018.
- Tadros R, Shakib S. Warfarin–indications, risks and drug interactions. Aust Fam Physician. 2010;39(7):476-479.
- Wasmer K, Eckardt L. Management of atrial fibrillation around the world: a comparison of current ACCF/AHA/HRS, CCS, and ESC guidelines. Europace. 2011;13(10):1368-1374.
- Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P; Authors/Task Force Members; Document Reviewers. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. European Heart Journal. 2016 Aug;18(8):891-975.
- Habib G, Badano L, Tribouilloy C, Vilacosta I, Zamorano JL, Galderisi M, Voigt JU, Sicari R, Cosyns B, Fox K, Aakhus S; European Association of Echocardiography. Recommendations for the practice of echocardiography in infective endocarditis. Eur J Echocardiogr. 2010;11:202-19.
- Habib G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta JP, Del Zotti F, Dulgheru R, El Khoury G, Erba PA, Iung B, Miro JM, Mulder BJ, Plonska-Gosciniak E, Price S, Roos-Hesselink J, Snygg-Martin U, Thuny F, Tornos Mas P, Vilacosta I, Zamorano JL. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015;36:3075-128.
- Lancellotti P, Tribouilloy C, Hagendorff A, Popescu BA, Edvardsen T, Pierard LA, Badano L, Zamorano JL; Scientific Document Committee of the European Association of Cardiovascular Imaging. Recommendations for the echocardiographic assessment of native valvular regurgitation: an executive summary from the European Association of Cardiovascular Imaging.Eur Heart J Cardiovasc Imaging. 2013;14:611-44.
- Lancellotti P, Price S, Edvardsen T, Cosyns B, Neskovic AN, Dulgheru R, Flachskampf FA, Hassager C, Pasquet A, Gargani L, Galderisi M, Cardim N, Haugaa KH, Ancion A, Zamorano JL, Donal E, Bueno H, Habib G. The use of echocardiography in acute cardiovascular care: recommendations of the European Association of Cardiovascular Imaging and the Acute Cardiovascular Care Association. Eur Heart J Cardiovasc Imaging. 2015;16:119-46.
- Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P; Authors/Task Force Members; Document Reviewers. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016 Aug;18(8):891-975.
- Chirillo F, Scotton P, Rocco F, Rigoli R, Borsatto F, Pedrocco A, De Leo A, Minniti G, Polesel E, Olivari Z. Impact of a multidisciplinary management strategy on the outcome of patients with native valve infective endocarditis. Am J Cardiol. 2013;112:1171–76.
- Hamirani YS, Dietl CA, Voyles W, Peralta M, Begay D, Raizada V. Acute aortic regurgitation. Circulation. 2012;126:1121-6.
- Kang DH, Kim YJ, Kim SH, Sun BJ, Kim DH, Yun SC, Song JM, Choo SJ, Chung CH, Song JK, Lee JW, Sohn DW. Early surgery versus conventional treatment for infective endocarditis. N Engl J Med. 2012;366:2466-73.
- Vital FM, Ladeira MT, Atallah AN. Non-invasive positive pressure ventilation (CPAP or bilevel NPPV) for cardiogenic pulmonary oedema. Cochrane Database Syst Rev. 2013 May 31;5:CD005351.”i>Essential Atlas of Heart Diseases.