Description
Course type: Online; Self-Paced
Specialty: Cardiology
Language: English
Resources: Debriefing Videos
Level: Intermediate
Target: Primary and Hospital Care Physicians
Modules: 10
Durations: 2 months
Time Effort: Up to 1 hour per module
Certificate: Yes
Course Description
Cardiac Arrhythmia can be defined as any abnormality in the rate, regularity, or sequence of cardiac activation. It can originate from abnormal impulse initiation in an individual myocyte or, more realistically, in a close cluster of myocytes.
Several mechanisms such as hypoxia, myocarditis, myocardial ischemia, or abnormal host immune response, which induce cardiac arrhythmias, have been described.
The principle of diagnosis in electrophysiology is to find the critical culprit anatomical site of the patient’s clinical arrhythmia.
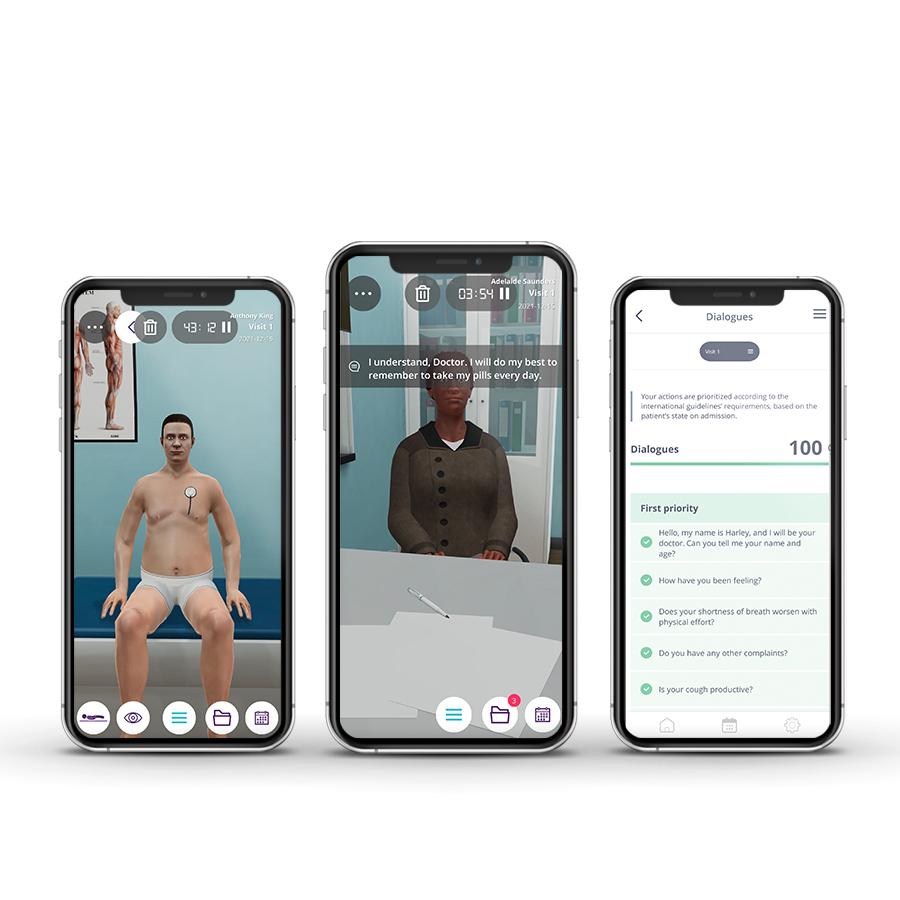
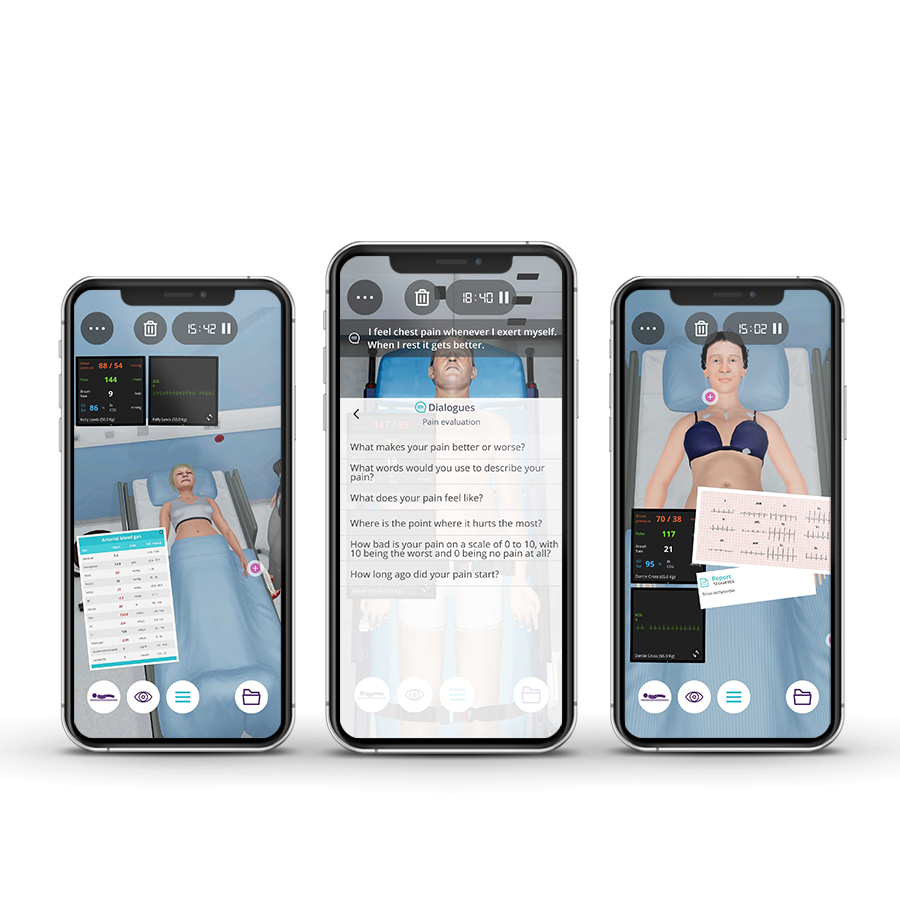
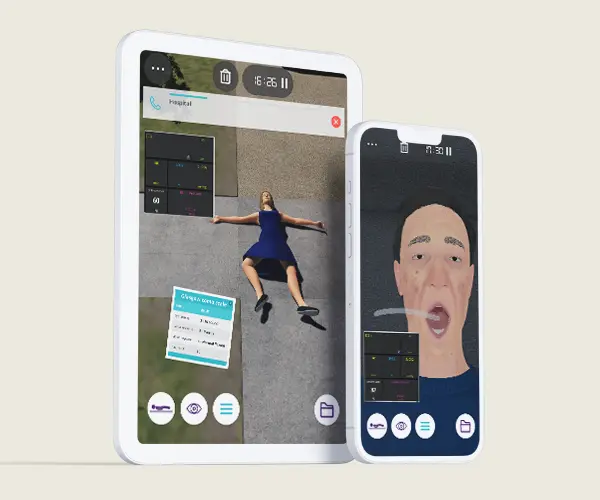
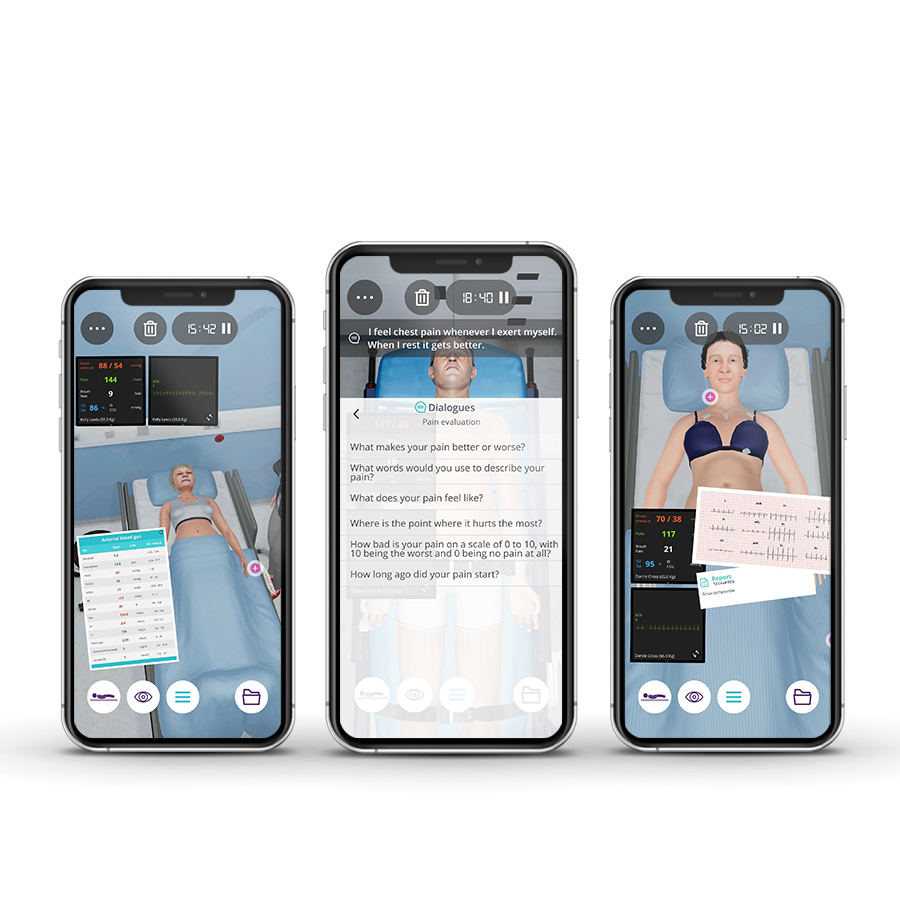
The SIM Beat course provides the knowledge and skills needed to interpret and treat cardiac arrhythmias, namely, Brady and Tachyarrhythmias in Emergency Room and Consultation environments.
The emphasis in this course is to practice,on virtual patients, rhythm interpretation, and appropriate treatment for chronic and life-threatening arrhythmias.
Course Overview
- 10 Modules
• The course consists of 10 modules, with each containing a Clinical Scenario. You can attempt each case up to 3 times. - Average Time to practice (per module)
• Clinical Scenario: 20 minutes per attempt (3 attempts: 60 minutes)
• Final attempt (if applicable): 20 minutes
• Multiple Choice Question: 5 minutes
• Feedback Area: 10 minutes
• Learning Objectives and Scientific References: 5 minutes
• Debriefing Video: 10 minutes - Online, Self-paced
• You have up to 2 months to complete the 10 modules at your own pace. The course can be accessed through Body Interact at any time. - Certificate of Completion
• After completing the course, you will receive a Certificate of Completion that can be added to your CV or Resume.
Learning Objectives
• Manage the non-valvular paroxysmal atrial fibrillation according to internationally accepted guidelines;
• Diagnose and treat ventricular arrhythmia and supraventricular tachycardia in several clinical settings;
• Define and deliver the best therapy for each arrhythmia.
Clinical Competencies
Safety
• Universal safety measures procedures
• Promote patient safety
Airway and Breathing
• Airway – naso/oropharyngeal
• Oxygen therapy (nasal cannula; non-rebreather; high-flow mask)
• Pulse oximetry
• Suctioning – upper airway
Circulation
• Cardiopulmonary resuscitation (CPR)
• Assess and interpret pulse (rate, rhythm and volume)
• Cardiac monitoring – 12-lead ECG
Medication- Routes
• Aerosolized / nebulized
• Intramuscular – auto-injector
• Intranasal – unit-dosed, premeasured
• Mucosal / Sublingual
• Oral
Module 1 – Catheter or Pill
Context: Symptoms including palpitations, fatigue, dizziness, dyspnoea, chest pain, and anxiety may be present in a cardiac arrhythmia. For each patient focus must be to identify the arrhythmia and deliver the best therapy to ensure clinical stability and optimal quality of life. This mainly includes drugs, lifestyle modifications, and state-of-the-art catheter-based therapies.
Virtual Scenario: Mr. Bradley had a heavily symptomatic atrial fibrillation crisis and went to the Emergency Department. He was discharged with a prescription consisting of a beta-blocker and a direct thrombin inhibitor, after undergoing successful cardioversion.
Module 2 – MI + 1
Context: How to approach De Novo Atrial Fibrillation? The focus must be set on ischemia and bleeding risk evaluation, eligibility for anticoagulation, and determining the best anti-arrytmic and risk factors therapy.
Virtual Scenario: Mr. Keith is going to have his first appointment for long-term health care management, after requiring emergency medical care due to a STEMI about four weeks ago.
Module 3 – A heart with bad rhythm
Context: Irregular heartbeats are a common complaint. How to address this symptom? How to value the Holter findings? Should we treat everyone? What is the best drug?
Virtual Scenario: Mrs. Walker arrives at the visit with many palpitations, some episodes of lightheadedness, fainting, and loss of consciousness with some days of evolution.
Module 4 – The machine that fixes the machine
Context: Pacemakers have complete change the cardiac arrhythmia landscape. However, they are not perfect. How to approach a pacemaker dysfunction?
Virtual Scenario: Ms. Craig has a past medical history of hypertension and dyslipidemia.
Module 5 – A Tale of two illnesses
Context: Patients with cardiac arrhythmias often have other cardiac diseases. Sometimes that disease triggers arrhythmias, sometimes arrhythmias trigger other cardiac diseases.
Virtual Scenario: Mr. Hale started to feel not well during a morning walk. His neighbor called for assistance as soon as he realized that Mr. Hale needed help.
Module 6 – No time to die?
Context: In extreme conditions, arrhythmias may lead to severe instability and even death. In this setting, we have to rapidly figure out what is happening and make sure that we stabilize the patient ASAP.
Virtual Scenario: Mr. Grey has always been healthy. However, one day he started feeling bad without apparent reason, and he didn’t get better the next day. He decided to go to the Emergency Department.
Module 7 – Fast and Furious
Context: VT is often a life-threatening condition. Clear judgment and fast decisions are paramount.
Virtual Scenario: Ms. Andresson was in her garden, doing some gardening when suddenly she felt her heart racing and had chest discomfort. She called the Emergency Department as soon as she could and was brought to the hospital.
Module 8 – Blackout
Context: Some AF patients may develop syncope and lightheadedness. In this setting ECG may show significant pauses, requiring a permanent device.
Virtual Scenario: Mrs. Smith was packing to go on a trip with her husband when she had a syncope. Her husband called for an ambulance.
Module 9 – One pacemaker, two pacemakers…three pacemakers?!
Context: What if the patient has not one but 2 pacemakers? This is good or bad? Does the patient need a third pacemaker?
Virtual Scenario: Mr. Abbott was at home with his wife when he had a syncope.
Module 10 – Is this love?
Context: Many arrhythmias present as palpitations, sometimes benign other times may lead to cardiac instability and severe quality of life impairment. How to approach and treat these clinical situations?
Virtual Scenario: Mr. Allen was at home with his son when he started feeling palpitations when he was at rest.
Authors and Speakers
With a multidisciplinary group of international clinical reviewers, Body Interact ensures a high standard of accuracy, diversity, and impact of its course.
Pedro Monteiro
MD, PhD
Faculty of Medicine, University of Coimbra, Portugal
Cardiology Consultant – Coimbra University Hospital
Scientific References
- 2019 Guidelines on Supraventricular Tachycardia (for the management of patients with). ESC Clinical Practice Guidelines.European Society of Cardiology. 2019
- Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS Guideline for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2017.
- Angiolillo DJ, Bhatt DL, Cannon CP, et al. Antithrombotic Therapy in Patients With Atrial Fibrillation Treated With Oral Anticoagulation Undergoing Percutaneous Coronary Intervention: A North American Perspective: 2021 Update. Circulation. 2021;143(6):583-596.
- Avezum A, Oliveira GB de F, Diaz R, et al. Efficacy and safety of dabigatran versus warfarin from the RE-LY trial. Open Heart. 2018;5(1):e000800.
- Bai Ying, Deng Hai, Shantsila Alena, Lip Gregory Y.H. Rivaroxaban Versus Dabigatran or Warfarin in Real-World Studies of Stroke Prevention in Atrial Fibrillation. Stroke. 2017;48(4):970-976.
- Berry Natalia C., Mauri Laura, Steg Philippe Gabriel, et al. Effect of Lesion Complexity and Clinical Risk Factors on the Efficacy and Safety of Dabigatran Dual Therapy Versus Warfarin Triple Therapy in Atrial Fibrillation After Percutaneous Coronary Intervention. Circulation: Cardiovascular Interventions. 2020;13(4):e008349.
- Brignole M. Recomendações para pacing cardíaco e terapêutica de ressincronização cardíaca. European Society of Cardiology. 2013-2015
- Brugada J, Katritsis DG, Arbelo E, et al. 2019 ESC guidelines for the management of patients with supraventricular tachycardia. The Task Force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC). European Heart Journal. 2020;41:655-720.
- Avezum Collet J-P, Thiele H, Barbato E, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). European Heart Journal. 2021;42(14):1289-1367.
- Cosentino F, Grant PJ, Aboyans V, et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: The Task Force for diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and the European Association for the Study of Diabetes (EASD). European Heart Journal. 2020;41(2):255-323.
- Glikson M, Nielsen JC, Kronborg MB, et al. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Europace. 2022;24(1):71-164.
- Hindricks G, Potpara T, Dagres N, et al. 2020 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS: The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42(5):373-498.
- Li X, Deitelzweig S, Keshishian A, et al. Effectiveness and safety of apixaban versus warfarin in non-valvular atrial fibrillation patients in “real-world” clinical practice. Thrombosis and Haemostasis. 2017;117(6):1072-1082.
- Avezum Lip Gregory Y.H., Keshishian Allison, Li Xiaoyan, et al. Effectiveness and Safety of Oral Anticoagulants Among Nonvalvular Atrial Fibrillation Patients. Stroke. 2018;49(12):2933-2944.
- Neumann F-J, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. European Heart Journal. 2019;40(2):87-165.
- Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). European Heart Journal. 2018;39(33):3021-3104.
- You JJ, Singer DE, Howard PA, et al. Antithrombotic therapy for atrial fibrillation: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e531S-75S.
- Zelniker TA, Ruff CT, Wiviott SD, et al. Edoxaban in atrial fibrillation patients with established coronary artery disease: Insights from ENGAGE AF–TIMI 48. European Heart Journal Acute Cardiovascular Care. 2019;8(2):176-185.