Description
Course type: Online; Self-Paced
Specialty: Internal Medicine
Language: English / Portuguese
Resources: Debriefing Videos
Level: Intermediate / Advanced
Target: Medical
Modules: 5
Durations: 2 months
Time Effort: Up to 110 minutes per module
Certificate: Yes
Course Description
Internal Medicine is a medical specialty that covers specialized medical care for the prevention, detection, and treatment of disease in adults. Internists apply scientific knowledge and clinical expertise to diagnose, treat, and care of adults. Physicians need to keep their knowledge up to date to improve the quality and effectiveness of healthcare.
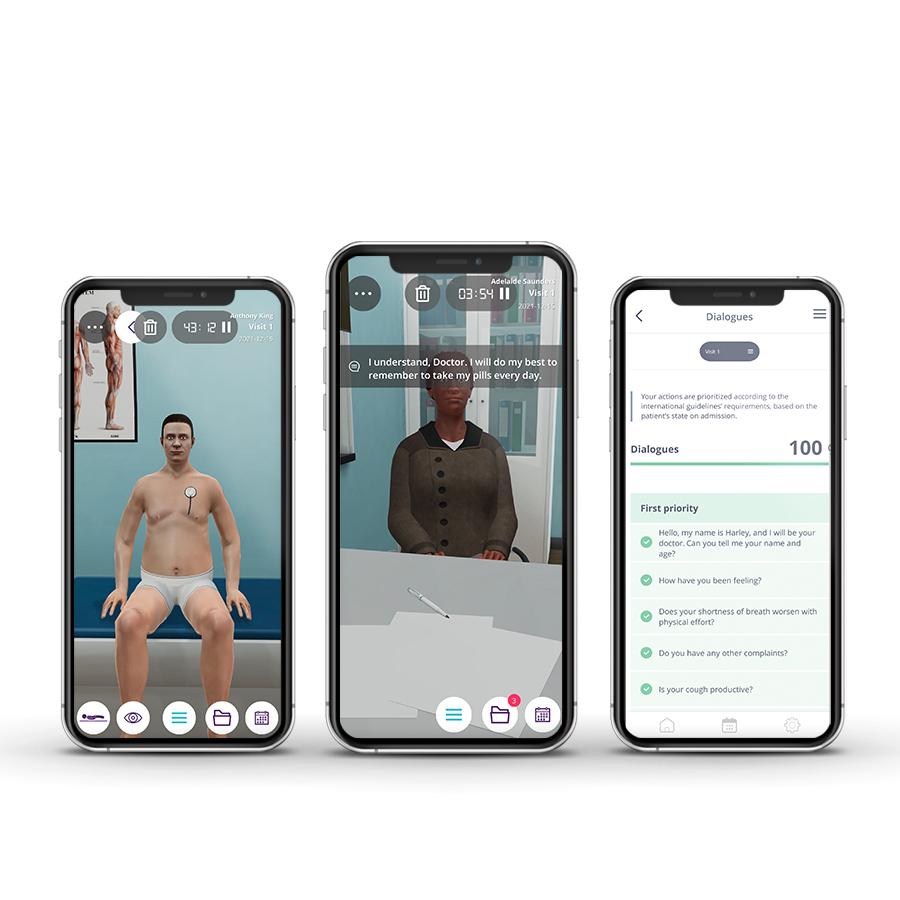
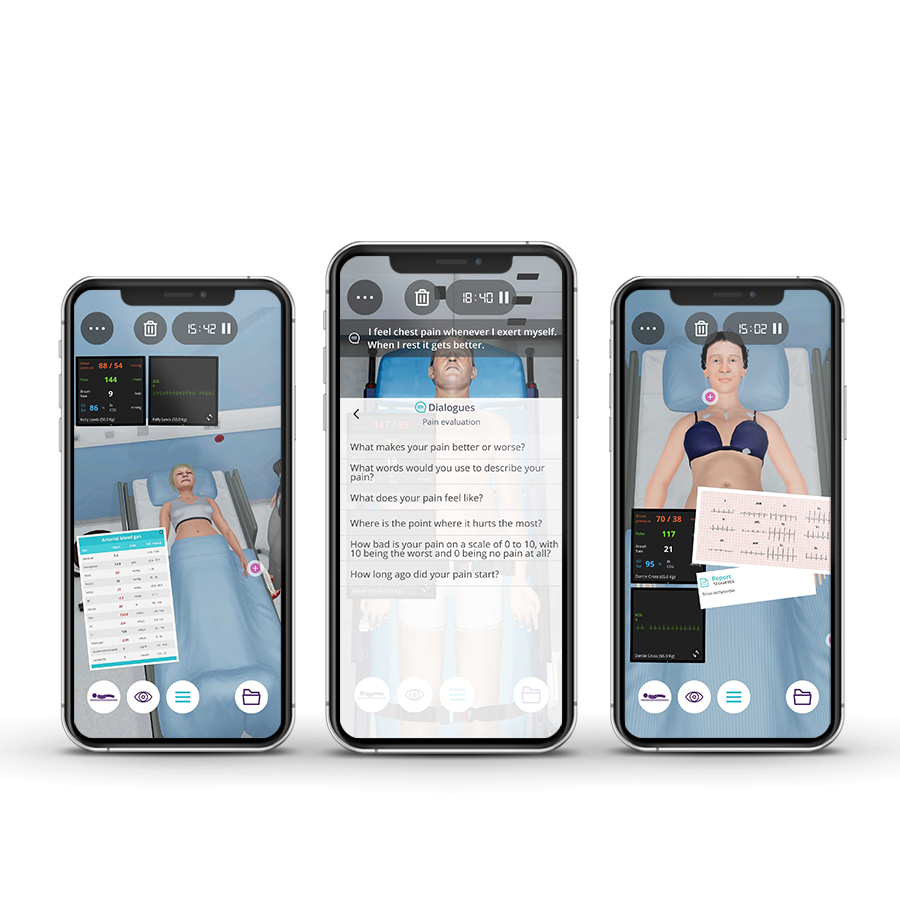
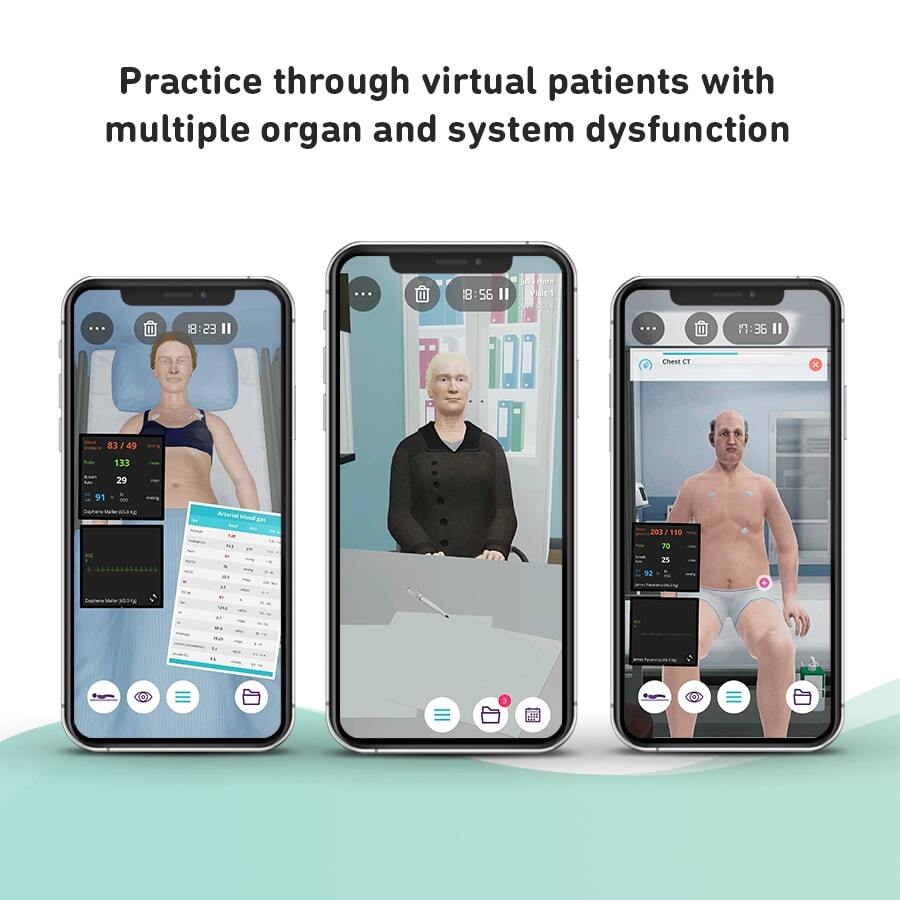
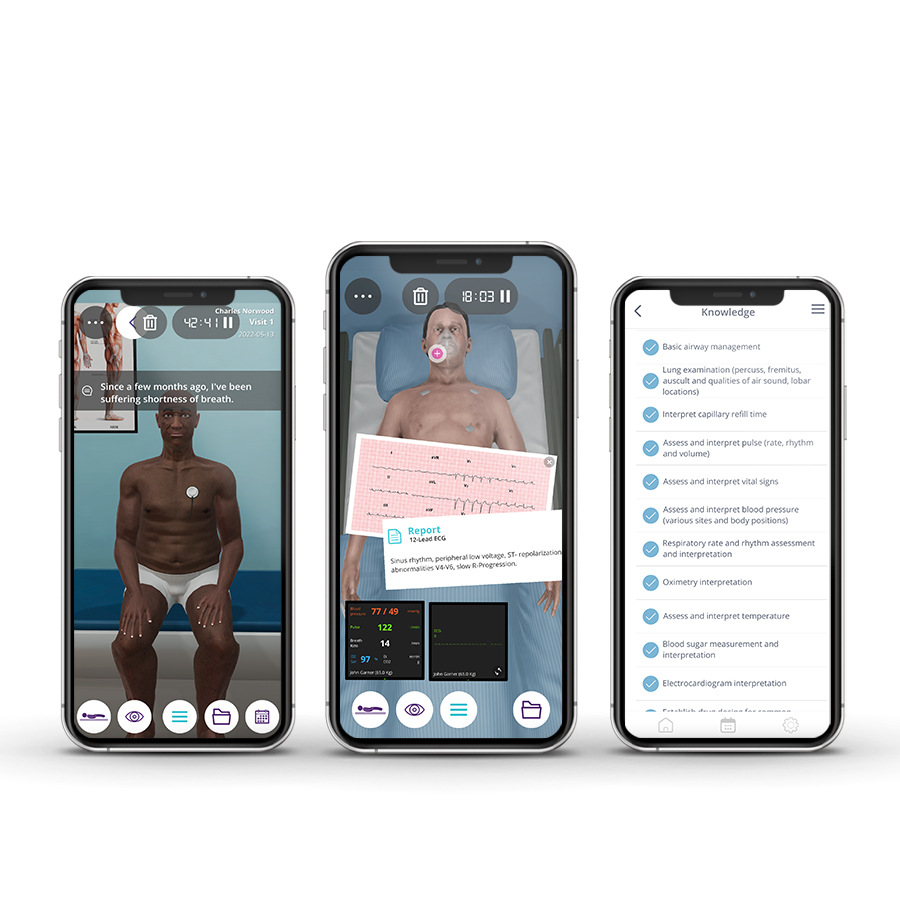
The Broad Practice of Internal Medicine course is designed to provide Internal Medicine specialists, with a simulated practice of five clinical scenarios with virtual patients in the Emergency and Consultation environment.
The clinical cases represent some of the most common problems encountered in clinical practice including the management of a variety of medical issues seen in gastroenterology, infectious diseases, cardiology, emergency medicine, and nephrology.
Course Overview
- 5 Modules
• 5 virtual patient cases of an intermediate level of complexity - Average Time to practice (per module)
• Clinical Scenario: 20 minutes per attempt (3 attempts: 60 minutes)
• Final attempt (if applicable): 20 minutes
• Multiple Choice Question: 5 minutes
• Feedback Area: 10 minutes
• Learning Objectives and Scientific References: 5 minutes
• Debriefing Video: 10 minutes - Online, Self-paced
• You have up to 2 months to complete the 10 modules at your own pace. The course can be accessed through Body Interact at any time. - Certificate of Completion
• After completing the course, you will receive a Certificate of Completion that can be added to your CV or Resume.
Learning Objectives
• Use medical knowledge to solve health problems related to the clinical practice of internal medicine
• Manage follow-up patients in the outpatient setting
• Identify and treat hypoperfusion and shock
• Detect and refer clinical cases that merit the attention of other specialists
Clinical Competencies
Safety
• Promote patient safety
• Collect patients clinical information
• Establish drug dosing for common medications and write prescriptions (including controlled drug)
Airway and Breathing
• Basic airway management
• Oximetry interpretation
• O2 administration
• Ventilator management
• Lung examination (percuss, fremitus, auscult and qualities of air sound, lobar locations)
• Detect heaves, thrills and sternal lift
Circulation
• Assess and interpret pulse (rate, rhythm and volume) and blood pressure
• Identify pulsus paradoxus
• Detect heart murmurs
• Identify S1 (tricuspid, mitral) and S2 (pulmonary, aortic) heart sounds and detect S3, S4 gallops
• Interpret capillary refill time
• Catheter management
Disability
• Blood sugar measurement and interpretation
• Urinalysis interpretation
• Abdominal examination (inspect, auscult, percuss and palp)
• Pupillary examination
• Assess mental status (level of arousal, response to auditory stimuli, to visual stimuli, noxious stimuli)
Exposure
• Assess and interpret temperature
• Interpretation of imaging tests (Chest x-ray, Ultrasonography, Computed tomography and Magnetic resonance imaging, Electrocardiogram interpretation, Nuclear imaging techniques…)
• Interpretation of lab tests (Liver function, Renal function, Fluid/Electrolyte, Cardiac enzyme, Hematocrit, Arterial Blood Gas, coagulopathy rate interpretation,Lipid test, Blood culture interpretation…)
• Cath lab techniques interpretation
• Recognize emergent situations – Illness severity assessment
• Refer to healthcare/ medical specialties
• Consultation management
• Nutrition management
• Hospital discharge
Module 1 – Missed last week’s dialysis session
Context: Dialysis is a treatment that allows the regulation of the extracellular volume and the elimination of elements such as potassium and urea, that accumulate during renal failure. Hemodialysis prolongs and improves the quality of life of patients with chronic renal failure.
Virtual Scenario: Mr. Paranzino is a dialysis patient, who has missed dialysis for the past week. He arrives at the emergency department at 02.30 on Saturday with shortness of breath and leg swelling.
Module 2 – Abdominal pain
Context: Taking the medical history and performing a physical examination are fundamental to diagnosing a disease. Since there are several conditions that lead to abdominal pain, the specific cause of the pain will determine the course of treatment.
Virtual Scenario: During the past four days, Daphne felt abdominal pain accompanied by nausea and vomiting. She has no diarrhea but has a fever. Today she decided to go to the emergency department.
Module 3 – Bloodstream infection
Context: The presence of a bacterium in the bloodstream may bring severe complications to the patient. Including hemodynamic complications and fever that require a systematic approach. The clinical variability and complexity of infections support the need for appropriate clinical judment regarding patient management.
Virtual Scenario: Sophia was brought to the emergency unit by her sons after they found her fallen with slurred speech. She was having regular cardiology visits.
Module 4 – Outpatient follow-up
Context: Patients with a history of heart disease need to be evaluated in order to improve their general and cardiovascular health, including improvement of their physical condition, exercise tolerance, and control of symptoms associated with the disease. Reducing cardiovascular risk factors reduces the potential for disease progression or recurrence.
Virtual Scenario: About a month ago, Julia required emergency medical care due to unstable angina. Today she has her first appointment for long-term health care management.
Module 5 – First follow-up appointment
Context: The medical assessment allows determining the patient’s state of health after having been hospitalized. It is essential to establish an adapted therapeutic and follow-up plan, in a coordinated and integrated way, in order to facilitate the maintenance of the capacity function and decrease the risk of re-hospitalization.
Virtual Scenario: A month ago, Mr. Paranzino was admitted to the hospital for evaluation of worsening dyspnea on exertion and leg swelling. Today is his first visit with you for long-term health care management.
Authors and Speakers
With a multidisciplinary group of international clinical reviewers, Body Interact ensures a high standard of accuracy, diversity, and impact of its course.
Paulo Martins
MD, PhD
Expert in Intensive Care
Faculty of Medicine, University of Coimbra, Portugal
Scientific References
- Abraham SC, Bhagavan BS, Lee LA, Rashid A, Wu TT. Upper gastrointestinal tract injury in patients receiving kayexalate (sodium polystyrene sulfonate) in sorbitol: clinical, endoscopic, and histopathologic findings. Am J Surg Pathol. 2001;25(5):637-644.
- Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC Guideline for the Management of Patients With Non–ST-Elevation Acute Coronary Syndromes – A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64(24):e139-e228.
- An JN, Lee JP, Jeon HJ, et al. Severe hyperkalemia requiring hospitalization: predictors of mortality. Crit Care. 2012;16(6):R225.
- Ash SR, Singh B, Lavin PT, et al. A phase 2 study on the treatment of hyperkalemia in patients with chronic kidney disease suggests that the selective potassium trap, ZS-9, is safe and efficient. Kidney Int. 2015;88(2):404-411.
- Bachert C, Chuchalin A, Eisebitt R, et al. Aspirin Compared with Acetaminophen in the Treatment of Fever And Other Symptoms of Upper Respiratory Tract Infection in Adults: A Multicenter, Randomized, Double-Blind, Double-Dummy, Placebo-Controlled, Parallel-Group, Single-Dose, 6-Hour Dose-Ranging Study. 6. . Clinical Therapeutics. 2005;27(7):993-1003.
- Baddour, LM, Wilson, WR, Bayer, AS, et al. (2015). Infective Endocarditis in Adults: Diagnosis, Antimicrobial Therapy, and Management of Complications. Circulation, 132(15), 1435-1486.
- Bakris GL, Pitt B, Weir MR, et al. Effect of Patiromer on Serum Potassium Level in Patients With Hyperkalemia and Diabetic Kidney Disease: The AMETHYST-DN Randomized Clinical Trial. JAMA. 2015;314(2):151-161.
- Brenner BM, Cooper ME, de Zeeuw D, et al. Effects of Losartan on Renal and Cardiovascular Outcomes in Patients with Type 2 Diabetes and Nephropathy. New England Journal of Medicine. 2001;345(12):861-869.
- Bushinsky DA, Williams GH, Pitt B, et al. Patiromer induces rapid and sustained potassium lowering in patients with chronic kidney disease and hyperkalemia. Kidney Int. 2015;88(6):1427-1433.
- Chaftari A, Hachem R, Mulanovich V, et al. Efficacy and safety of daptomycin in the treatment of Gram-positive catheter-related bloodstream infections in cancer patients. International Journal of Antimicrobial Agents. 2010;36(2):182-186.
- Chernin G, Gal-Oz A, Ben-Assa E, et al. Secondary Prevention of Hyperkalemia With Sodium Polystyrene Sulfonate in Cardiac and Kidney Patients on Renin-Angiotensin-Aldosterone System Inhibition Therapy. Clin Cardiol. 2012;35(1):32-36.
- Collins AJ, Reaven N, Funk S, et al. Potassium Levels and Mortality in Patients with CKD. Poster presented at: American Society of Nephrology Kidney Week 2014; November 11-16, 2014; Philadelphia, PA. Poster TH-PO705.
- Cubicin®. Summary of Product Characteristics. 2014.
- Dandache P, Aronow WS, Sakoulas G. Clinical Update on the Diagnosis and Treatment of Bacterial Endocarditis. Comprehensive Therapy. 2007;33(4):192-207.
- Desai AS, Swedberg K, McMurray JJV, et al. Incidence and Predictors of Hyperkalemia in Patients With Heart Failure: An Analysis of the CHARM Program. Journal of the American College of Cardiology. 2007;50(20):1959-1966.
- Drawz PE, Babineau DC, Rahman M. Metabolic Complications are Common in Elderly Patients with Chronic Kidney Disease. J Am Geriatr Soc. 2012;60(2):310-315.
- Einhorn LM, Zhan M, Hsu VD, et al. The frequency of hyperkalemia and its significance in chronic kidney disease. Arch Intern Med. 2009;169(12):1156-1162
- Grundy Scott M., Stone Neil J., Bailey Alison L., et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA /AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol. Circulation. 0(0):CIR.0000000000000625.
- Healthcare Cost and Utilization Project (HCUP). https://www.ahrq.gov/research/data/hcup/index.html. Accessed April 12, 2017.
- Hernandez G, Bruhn A, Romero C, et al. Management of septic shock with a norepinephrine-based haemodynamic algorithm. Resuscitation. 2005;66(1):63-69.
- Kasner SE, Wein T, Piriyawat P, et al. Acetaminophen for Altering Body Temperature in Acute Stroke A Randomized Clinical Trial. Stroke. 2002;33(1):130-135.
- Kasper D, Fauci A, Hauser S, Longo D, Jameson JL, Loscalzo J. Harrison’s Principles of Internal Medicine. 19th Ed. New York, NY: McGraw-Hill; 2015.
- Khanna A, White WB. The management of hyperkalemia in patients with cardiovascular disease. Am J Med. 2009;122(3):215-221
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO Clinical Practice Guideline for the Management of Blood Pressure in Chronic Kidney Disease. Kidney Int Suppls. 2012;2(5):337-414.
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppls. 2013;3:1-150.
- Laupland KB. Fever in the critically ill medical patient: Critical Care Medicine. 2009;37(Supplement):S273-S278.
- Liu C, Bayer A, Cosgrove SE, et al. Clinical Practice Guidelines by the Infectious diseases Society of america for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clinical Infectious Diseases. 2011;52(1):285-292.
- Murray KP, Zhao JJ, Davis SL, et al. Early Use of Daptomycin Versus Vancomycin for Methicillin-Resistant Staphylococcus aureus Bacteremia With Vancomycin Minimum Inhibitory Concentration >1 mg/L: A Matched Cohort Study. Clinical Infectious Diseases. 2013;56(11):1562-1569.
- Nathwani D, Morgan M, Masterton RG, et al. Guidelines for UK practice for the diagnosis and management of methicillin-resistant Staphylococcus aureus (MRSA) infections presenting in the community. Journal of Antimicrobial Chemotherapy. 2008;61(5):976-994.
- Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease. Circulation. June 2014.
- Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. June 2017.
- Pitt B, Collins A, Reaven N, et al. Effect of cardiovascular comorbidities on the mortality risk associated with serum potassium. Poster presented at: American Heart Association 2014 Scientific Sessions; November 15-19, 2014; Chicago, IL. Poster 2443.
- Rhodes A, Evans LE, Alhazzani W, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2016. Critical Care Medicine. 2017;45(3):486.
- Rydén L, Grant PJ, Anker SD, et al. ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. European Heart Journal. 2013;34(39):3035-3087
- Sterns RH, Grieff M, Bernstein PL. Treatment of hyperkalemia: something old, something new. Kidney International. 2016;89(3):546-554.
- Soriano A, Marco F, Martínez JA, et al. Influence of Vancomycin Minimum Inhibitory Concentration on the Treatment of Methicillin-Resistant Staphylococcus aureus Bacteremia. Clinical Infectious Diseases. 2008;46(2):193-200.15.
- Weir MR, Bakris GL, Bushinsky DA, et al. Patiromer in Patients with Kidney Disease and Hyperkalemia Receiving RAAS Inhibitors. New England Journal of Medicine. 2015;372(3):211-221.
- Weisberg LS. Management of severe hyperkalemia. Crit Care Med. 2008;36(12):3246-3251.
- Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021-3104.
- You JJ, Singer DE, Howard PA, et al. Antithrombotic Therapy for Atrial Fibrillation: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. CHEST. 2012;141(2):e531S-e575S.