Description
Course type: Online; Self-Paced
Specialty: Specialty: Emergency Medicine
Language: English
Resources: Debriefing Videos
Level: Basic / Intermediate
Target: Medical
Modules: 6
Durations: 2 months
Time Effort: Up to 110 minutes per module
Certificate: Yes
Course Description
The electrocardiogram (ECG/EKG) is one of the first complementary diagnostic tests to be used in numerous clinical situations. Through it, it is possible to diagnose and adapt the treatment. This auxiliary diagnostic tool has been presented as a fundamental test, sometimes essential, in the Medicine area, whether in Hospital or in Primary Care.
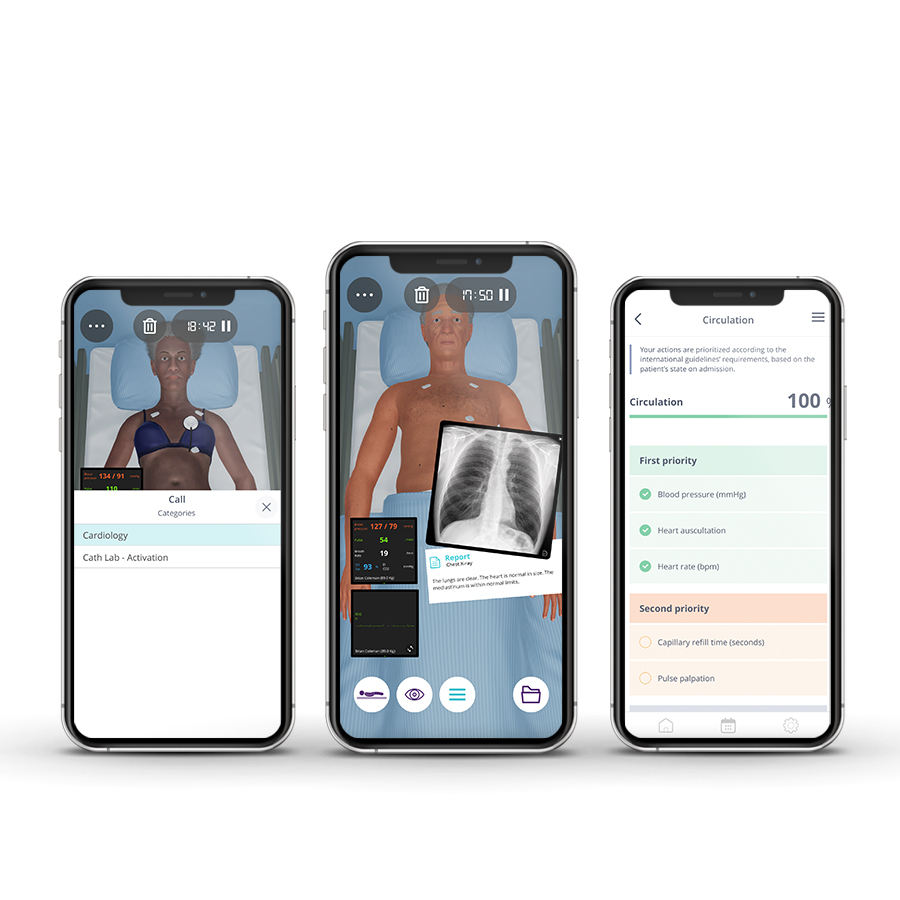
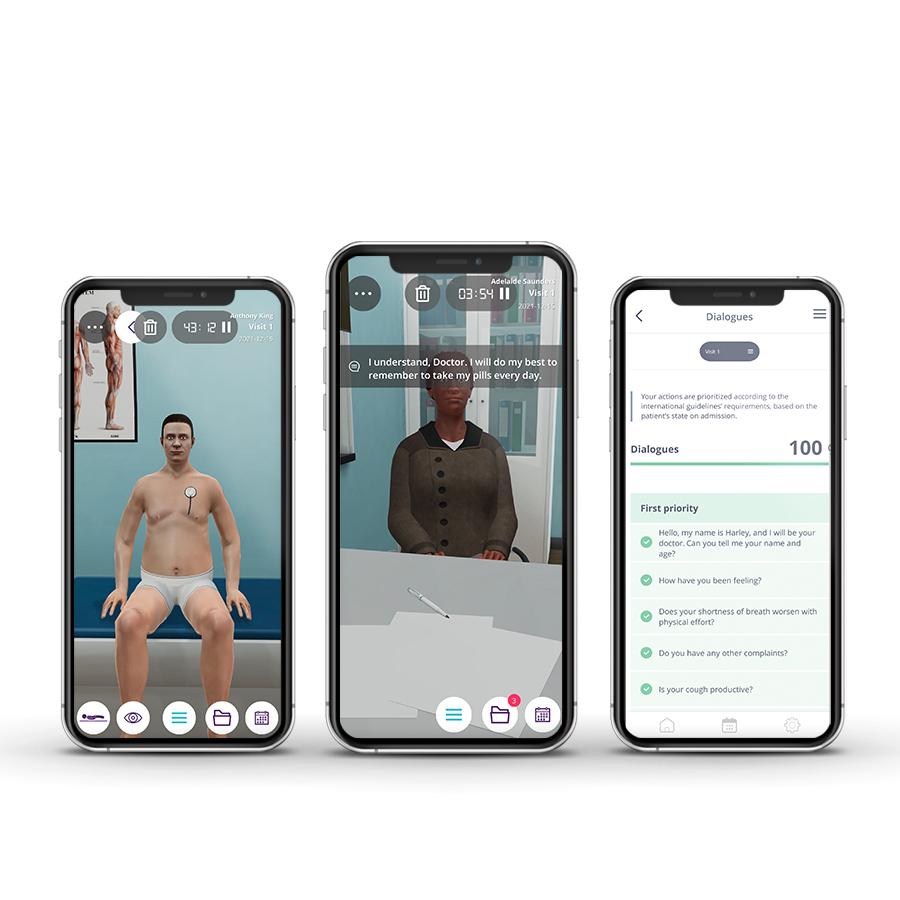
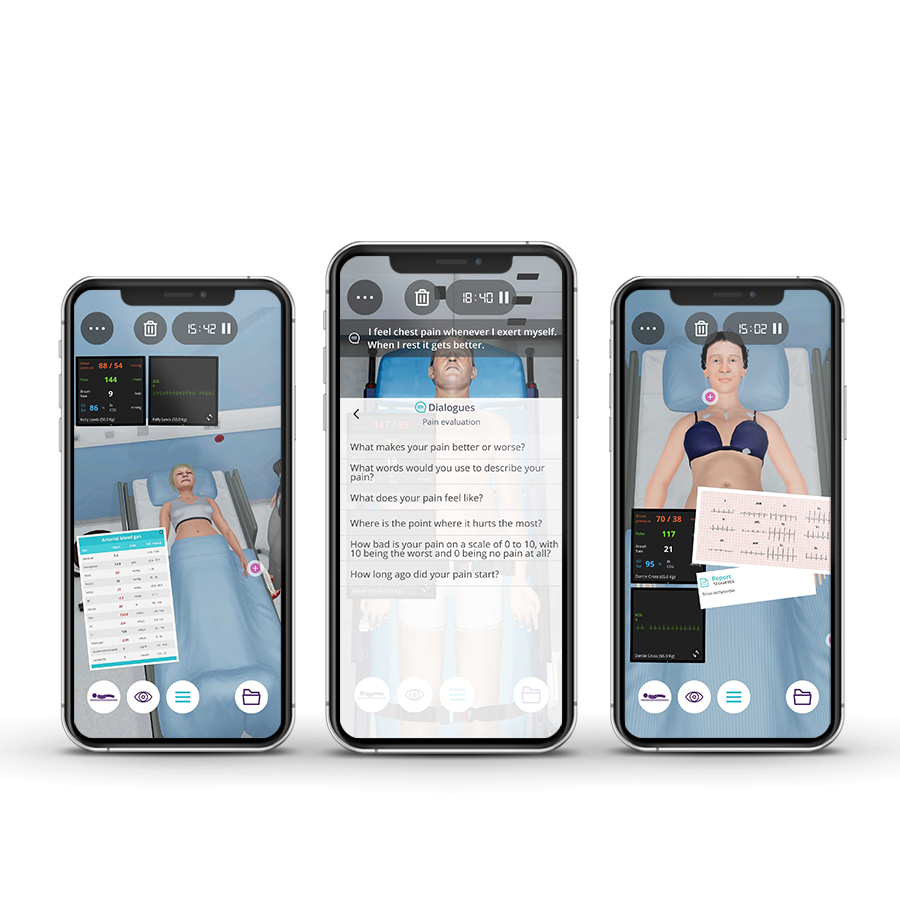
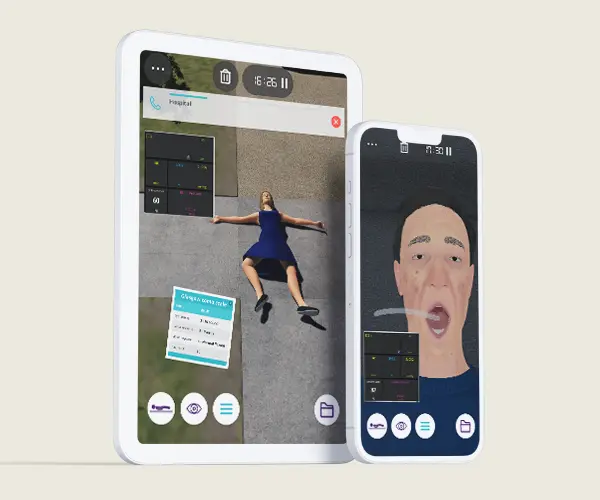
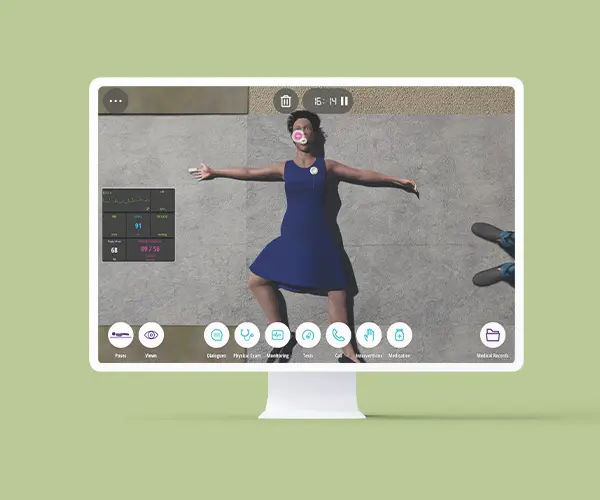
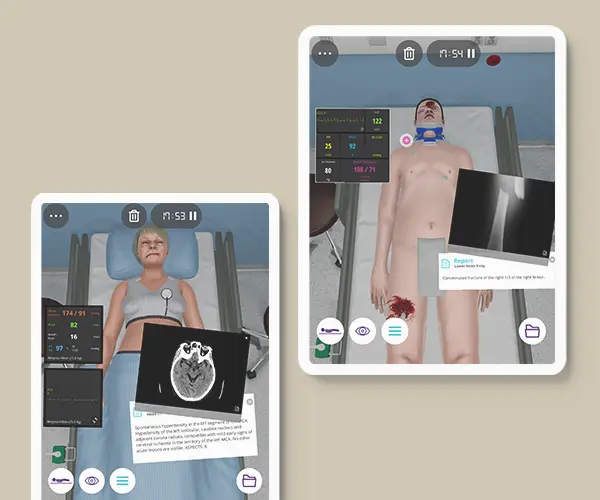
The Challenges in Electrocardiography course through the Body Interact advanced medical simulation technology allows the professional to identify cardiac clinical situations by applying the appropriate care and treatments in the shortest time possible, providing safe and quality care through virtual patients.
Course Overview
- 6 Modules
• 6 virtual patient cases of an intermediate level of complexity - Average Time to practice (per module)
• Clinical Scenario: 20 minutes per attempt (3 attempts: 60 minutes)
• Final attempt (if applicable): 20 minutes
• Multiple Choice Question: 5 minutes
• Feedback Area: 10 minutes
• Learning Objectives and Scientific References: 10 minutes
• Debriefing Video: 10 minutes - Online, Self-paced
• You have up to 2 months to complete the 6 modules at your own pace. The course can be accessed through Body Interact at any time. - Certificate of Completion
• After completing the course, you will receive a Certificate of Completion that can be added to your CV or Resume.
Learning Objectives
• Identify variants of the normal, early repolarization, respiratory sinus dysrhythmia, and lead misplacement
• Identify cardiac rhythms with normal and slow rates
• Identify atrioventricular and intraventricular conduction abnormalities.
• Develop clinical reasoning of myocardial infarction through the patient’s clinical history
• Identify what ECG changes might myocardial ischemia cause other than ST-segment elevation and what are the differential diagnoses of these changes
• Identify electrocardiographic indications for reperfusion therapy
Clinical Competencies
Safety
• Universal safety measures procedures
• Collect patients clinical information
• Establish drug dosing for common medications
Airway and Breathing
• Basic airway management;
• Airway suctioning
• Respiratory rate and rhythm assessment
• Oximetry interpretation
Circulation
• Assess and interpret pulse (rate, rhythm and volume) and blood pressure (various sites and body positions)
Disability
• Mental status assessment (level of arousal, response to auditory stimuli, to visual stimuli, noxious stimuli)
Exposure
• Assess and interpret temperature
• Hand and foot examination
• Wound care and lesion qualities assessment (petechiae, urticaria, jaundice, vesicles, etc)
•Handle and position patients body
• Refer to healthcare/ medical specialties
• Contribute to the implementation of physiotherapy interventions
Module 1 – Felt bad at home
Context: The standard 12-lead electrocardiogram is a representation of the heart’s electrical activity recorded from electrodes on the body surface. When interpreted accurately, an ECG can detect and monitor a host of heart conditions – from arrhythmias to coronary heart disease to electrolyte imbalance.
Virtual Scenario: Ms. Moyo was at home with his grandmother, when she started feeling palpitations and anxiety. Her grandmother tries to understand what is happening with her, but she just mentions that she’s not feeling well.
Module 2 – Bicycle fall
Context: The existence of electrocardiographic variants may be common in individuals with a structurally normal heart, more frequent in males, in blacks, in younger (less than 40 years old), and more athletically active individuals with characteristics that predispose them to vagotonia. However, it is very important to make a differential diagnosis of pathologies that could be fatal, such as Acute Myocardial Infarction.
Virtual Scenario: Mr. Dean was on a bicycle marathon race when he suddenly, on a curve, fell and broke his leg. He was stabilized at the scene and, after that, immediately brought to the Emergency Department.
Module 3 – Faint in the garden
Context: The ECG is an important tool, inexpensive and easy to perform, that may allow you to identify various causes of syncope. it can also be used to help predict prognosis and risk-stratify patients.
Virtual Scenario: Mr. Waters was walking his dog outside when suddenly felt chest palpitations and fainted in the garden. His sister called for an ambulance.
Module 4 – Unspecified malaise
Context: Sometimes, the strange appearance of the ECG, either by the appearance of its waves or by the duration of the intervals, does not allow immediate identification of the underlying disorder. Knowledge of electrical and mechanical cardiac physiology is essential.
Virtual Scenario: Mr. Finn is a gardener. Lately, he has been feeling down, with some family problems and also at work.
Module 5 – Edema of the lower limbs
Context: Lower limb edema is a clinical sign that may translate into an abnormality of the heart function. Knowledge of the patterns of clinical presentation together with electrocardiographic imaging may contribute to the diagnosis of cardiac pathology.
Virtual Scenario: Mr. Coleman has a personal history of heart failure, atrial fibrillation, hypertension, and obesity. He is retired and works only in agriculture, living with his wife.
Module 6 – Chest pain
Context: Chest pain affects 20% to 40% of the general population. In many cases, it is related to heart problems. A quick diagnosis and a correct approach can save lives.
Virtual Scenario: Ms. Harris is a journalist and has been under tremendous stress and anxiety with deadlines to deliver some important articles. This evening she felt a pain in her chest and decided to come to the emergency room.
Authors and Speakers
With a multidisciplinary group of international clinical reviewers, Body Interact ensures a high standard of accuracy, diversity, and impact of its course.
Paulo Martins
Cardiopneumologist / Clinical Physiologist
North Lisbon University Hospital Centre, Portugal (CHULN)
Paulo Martins
MD, PhD
Expert in Intensive Care
Faculty of Medicine, University of Coimbra, Portugal
Scientific References
- Ali A, Butt N, Sheikh AS. Early repolarization syndrome: A cause of sudden cardiac death. World J Cardiol. 2015;7(8):466-475.
- Bernath P, Kusumoto F. ECG interpretation for everyone. 1st ed. Wiley-Blackwell; 2012.
- Borja I, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). European Heart Journal. 2018; 39 (2): 119–177.
- Brady W, Hudson K, et al. The ECG in Prehospital Emergency Care. Wiley-Blackwell; 2013.
- Brignole M, Moya A, de Lange FJ, et al. 2018 ESC Guidelines for the diagnosis and management of syncope. European Heart Journal. 2018;39(21):1883-1948.
- Cai Q, Mehta N, Sgarbossa EB, et al. The left bundle-branch block puzzle in the 2013 ST-elevation myocardial infarction guideline: from falsely declaring emergency to denying reperfusion in a high-risk population. Are the Sgarbossa Criteria ready for prime time? Am Heart J. 2013;166(3):409-413.
- Hindricks G, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. European Heart Journal. 2021; 42 (5): 373–498.
- Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, et al. 2018 ACC/AHA/HRS guideline on the evaluation and management of patients with bradycardia and cardiac conduction delay: a report of the ACC/AHA Task Force on Clinical Practice Guidelines and the HRS. Circulation. 140:e382-e482; 2019.
- Loscalzo J. Harrison’s Cardiovascular Medicine. 3th ed. McGrawHill; 2010.
- Lynch R. ECG lead misplacement: A brief review of limb lead misplacement. African Journal of Emergency Medicine. 2014;4(3):130-139.
- Metkus T. ECG Rounds. McGrawHill; 2014.
- Morgan, E. All About HRV Part 4: Respiratory Sinus Arrhythmia – MindWare Technologies Support. Accessed November 5, 2021.
- Oldroyd SH, Quintanilla Rodriguez BS, Makaryus AN. First Degree Heart Block. In: StatPearls. StatPearls Publishing; 2021.
- Patton Kristen K., Ellinor Patrick T., Ezekowitz Michael, et al. Electrocardiographic Early Repolarization. Circulation. 2016;133(15):1520-1529