Description
Course type: Online; Self-Paced
Specialty: Internal Medicine
Language: English / Portuguese
Resources: Debriefing Videos
Level: Intermediate / Advanced
Target: Medical
Modules: 5
Durations: 2 months
Time Effort: Up to 110 minutes per module
Certificate: Yes
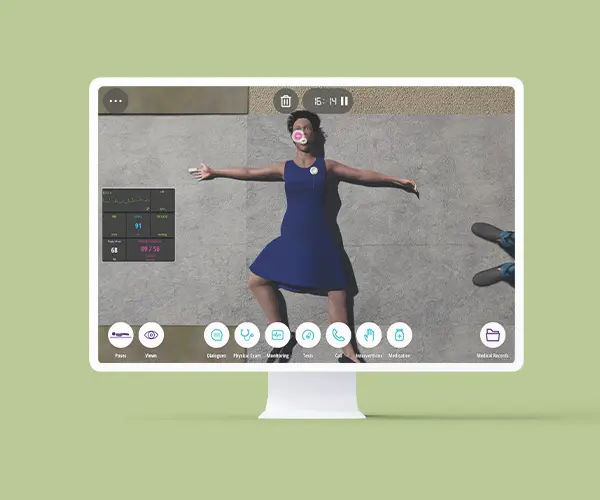
Course Description
Emergency Medicine (EM) is a medical specialty in which patients present with emerging medical and surgical problems that are sometimes life-threatening.
The practice of medicine in an emergency department or urgent care setting requires the constant incorporation and application of new knowledge. Emergency physicians are first-line providers of emergency care in which timely diagnosis and treatment contribute to a better prognosis for the patient.
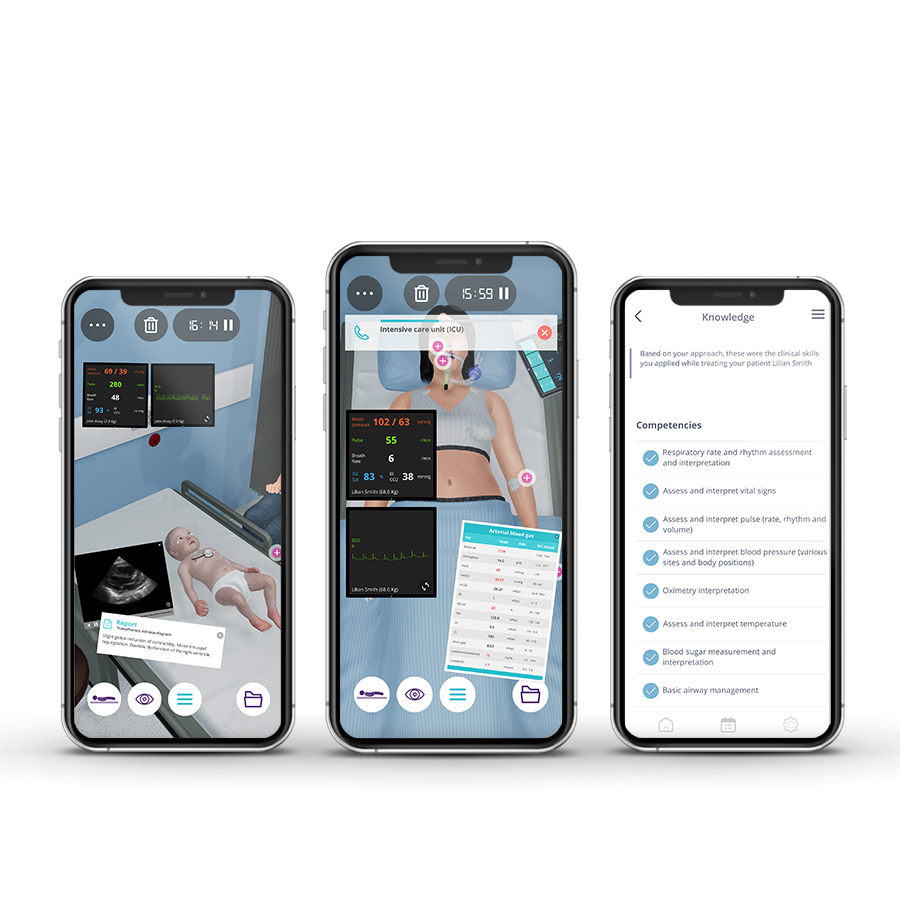
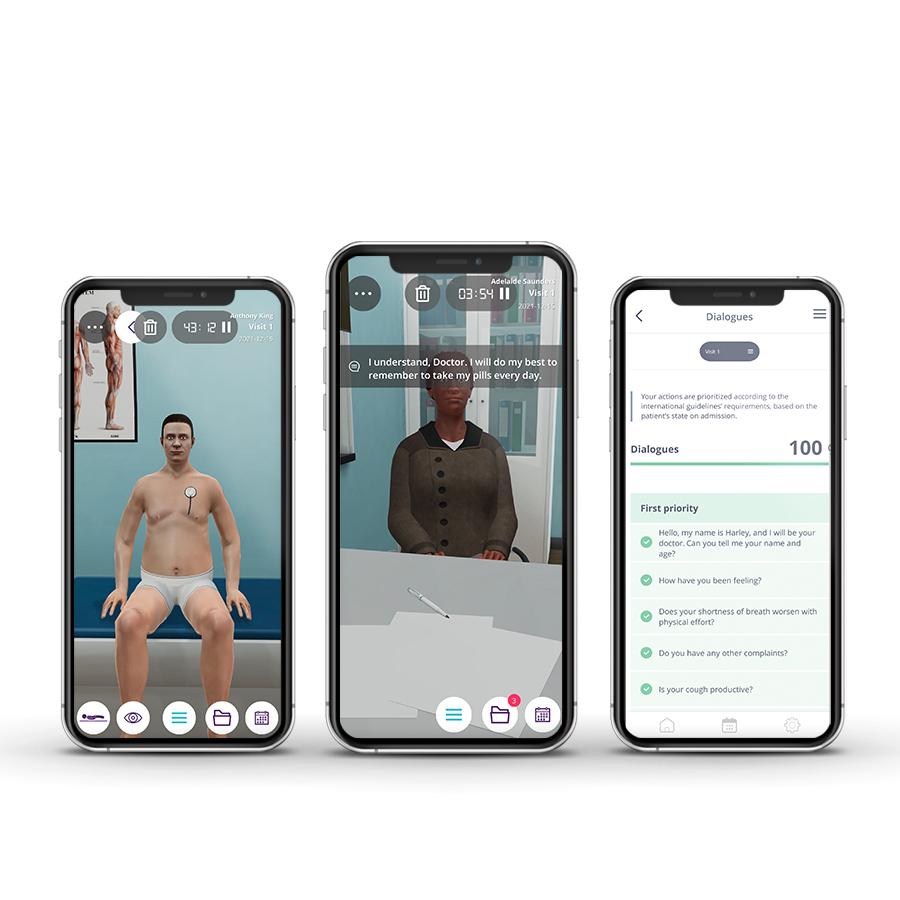
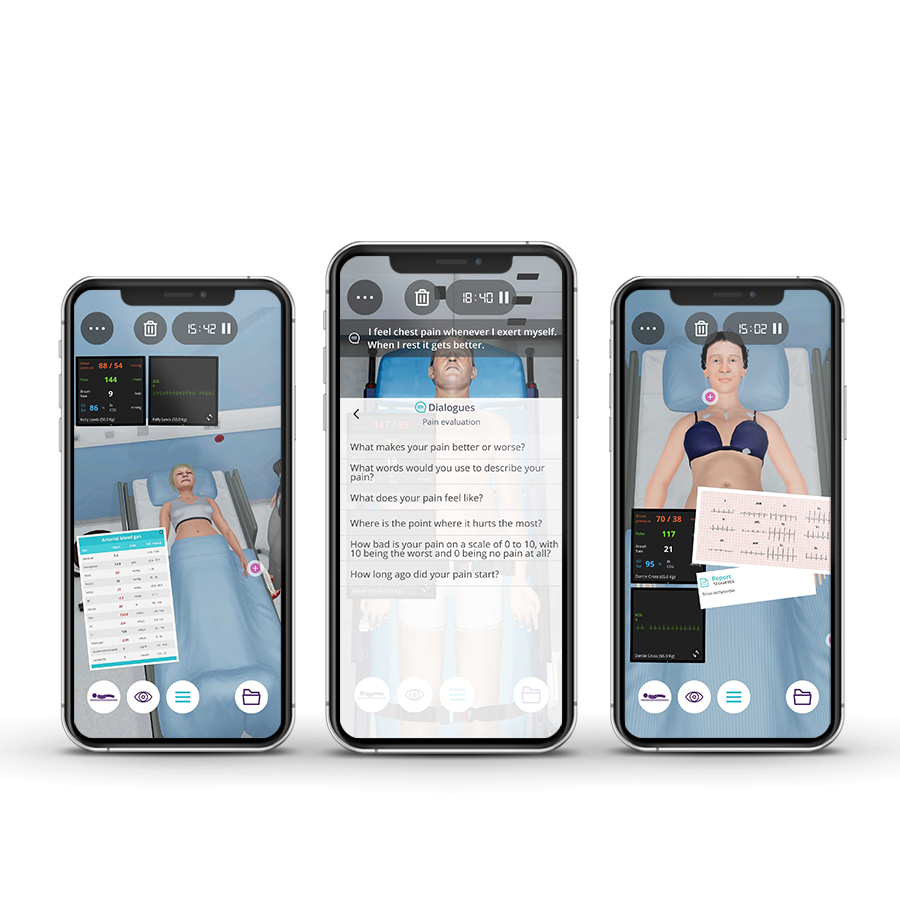
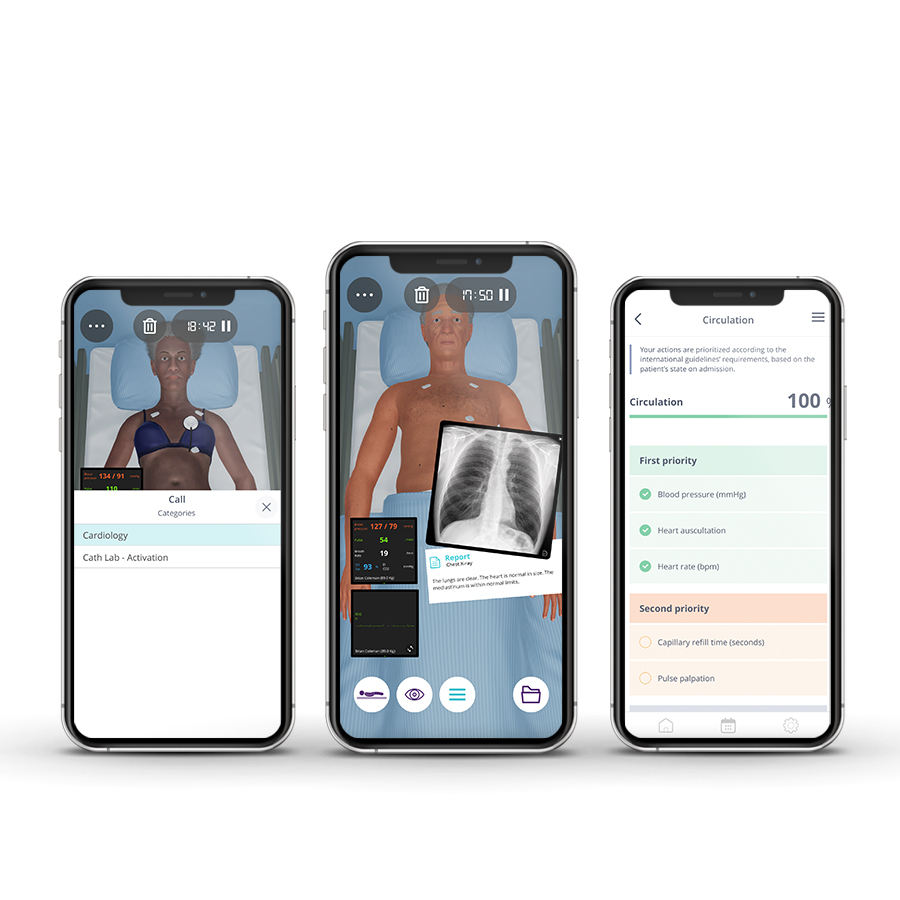
The Emergency and Urgent Medical Care course enables emergency physicians to manage acute patients, covering current guidelines to ensure the most up-to-date care. This course allows addressing various clinical conditions in the vast areas of Trauma, Toxicology, Pediatrics, and Critical Care.
Course Overview
- 5 Modules
• 5 virtual patient cases of an intermediate level of complexity - Average Time to practice (per module)
• Clinical Scenario: 20 minutes per attempt (3 attempts: 60 minutes)
• Final attempt (if applicable): 20 minutes
• Multiple Choice Question: 5 minutes
• Feedback Area: 10 minutes
• Learning Objectives and Scientific References: 5 minutes
• Debriefing Video: 10 minutes - Online, Self-paced
• You have up to 2 months to complete the 10 modules at your own pace. The course can be accessed through Body Interact at any time. - Certificate of Completion
• After completing the course, you will receive a Certificate of Completion that can be added to your CV or Resume.
Learning Objectives
• Identify the first-line priorities of assessment and treatment of any critically ill or injured patient
• Perform initial evaluation, stabilization, and management of patients with clinical problems commonly encountered in the Emergency Department
• Rapidly recognizing acute life- or limb-threatening illnesses or injuries
• Perform a systematic approach to resuscitation and stabilization of medical, surgical, and traumatic emergencies
Clinical Competencies
Safety
• Universal safety measures procedures
• Promote patient safety
• Establish drug dosing for common medications
Airway and Breathing
• Basic airway management
• Placement of oral airway
• Respiratory rate and rhythm assessment and interpretation
• Oximetry interpretation
• O2 administration
• Thorax (shape, movement, diameter, ribs and diaphragm)
• Lung (percuss, fremitus, auscult and qualities of air sound, lobar locations) examination
•Ventilator management
• Managing and interpreting chest drainage tubes
Circulation
• Assess and interpret pulse (rate, rhythm and volume) and blood pressure
• Interpret capillary refill time
• Catheter management
• Determinate patient’s blood type and manage its component
• Cardiac defibrillation
Disability
• Assess mental status (level of arousal, response to auditory stimuli, to visual stimuli, noxious stimuli)
• Measure and interpret blood sugar values
• Detect heart murmurs and identify S1 (tricuspid, mitral) and S2 (pulmonary, aortic) heart sounds and detect S3, S4 gallops
Exposure
• Lesion qualities assessment (petechiae, urticaria, jaundice, vesicles, etc)
• Gait, station and proprioception assessment
• Muscle tone, bulk, strength assessment
• Perform abdominal and pelvic examination (inspect, auscult, percuss and palp)
• Recognize the indications to perform gastric lavage
• Interpret imaging tests (Chest x-ray, Ultrasonography, Computed tomography and Magnetic resonance imaging, Electrocardiogram interpretation, Nuclear imaging techniques, Abdominal ultrasound)
• Interpret lab tests (Liver function, Renal function, Fluid/Electrolyte, Cardiac enzyme, Hematocrit, Arterial Blood Gas, coagulopathy rate,Lipid test, Blood culture, Urinalysis)
• Bladder catheterization (male and female)
• Perform body immobilization
• General wound care
• Back examination
Module 1 – Gun shot
Context: All injuries produce direct tissue damage. It’s nature and extent depend on the anatomical site, mechanism, and intensity. Severe direct tissue injuries on critical organs account for the majority of immediate trauma deaths.
Virtual Scenario: Lucas was working on building a house when he was hit by a stray bullet in a gang brawl. He was brought to the emergency department.
Module 2 – Slurred speech
Context: Identifying symptoms that may be associated with unknown medical conditions is essential to approach the patient as soon as possible, and to understand their cause in order to avoid severe complications. Some symptoms are immediate, while others may appear later.
Virtual Scenario: Lilian was found at home by her brother in her bedroom confused, dull with slurred speech.
Module 3 – Car accident
Context: Road accidents are one of the main causes of mortality and morbidity worldwide. An adequate systematized approach contributes to the reduction of severe complications.
Virtual Scenario: Jack was involved in a car collision with a motorbike, but can’t recall what happened. Due to the severity of injuries including seat belt abrasions, multiple contusions, and spine immobilization, he was carried out at the scene.
Module 4 – Easily irritable baby
Context: Identifying the cause of a baby’s crying can be challenging. It can be associated with serious conditions. Its rapid assessment and timely medical management can lead to better clinical outcomes and increase the survival rate of pediatric patients.
Virtual Scenario: John is a healthy baby who just recently passed eight months of age. However, one day he started crying without apparent reason, and he didn’t get better the next day, so his mother brought him to the Pediatric Emergency Unit.
Module 5 – Difficulty breathing
Context: Shortness of breath can be associated with severe and potentially fatal clinical conditions, if not treated in a timely manner. Identifying the cause is critical for proper and effective treatment.
Virtual Scenario: Ms. Hughes was celebrating a friend’s birthday at a dinner party when suddenly she started with respiratory difficulty, and wheezing became progressively more severe. Her friend called for an ambulance, reporting that she is allergic to seafood and had eaten a little cocktail, not knowing that it had seafood
Authors and Speakers
With a multidisciplinary group of international clinical reviewers, Body Interact ensures a high standard of accuracy, diversity, and impact of its course.
Paulo Martins
MD, PhD
Expert in Intensive Care
Faculty of Medicine, University of Coimbra, Portugal
Scientific References
- Al-Koudmani I, Darwish B, Al-Kateb K, Taifour Y. Chest trauma experience over eleven-year period at Al-Mouassat University Teaching Hospital – Damascus: a retrospective review of 888 cases. J Cardiothorac Surg. 2012; 7(1):35
- Aukema TS, Beenen LFM, Hietbrink F, Leenen LPH. Initial assessment of chest x-ray in thoracic trauma patients: awareness of specific injuries. Word J Radiol. 2012; 4(2):48-52.
- Baud F, Garnier, R. Toxicologie clinique. 6th ed. Lavoisier Medécin; 2017.
- Biffl WL, Kaups KL, Pham TN, et al. Validating the Western Trauma Association algorithm for managing patients with anterior abdominal stab wounds: a Western Trauma Association multicenter trial. J Trauma. 2011;71(6):1494-1502.
- Brown CA 3rd, Bair AE, Pallin DJ, et al. Techniques, success, and adverse events of emergency department adult intubations. Ann Emerg Med 2015; 65:363.
- Cicardi M, Aberer W, Banerji A, et al. Classification, diagnosis, and approach to treatment for angioedema: consensus report from the Hereditary Angioedema International Working Group. Allergy 2014; 69:602.
- Committee on Trauma, American College of Surgeons. National Trauma Data Bank Annual Report 2014. Chicago: American College of Surgeons; 2014.
- Coumoul X, Andujar P, Baeza-Squiban A, et al. Toxicologie. Dunod; 2017.
- Flerlage J, Engorn B. The Harriet Lane Handbook – a Manual for Pediatric House Officers. Philadelphia, PA: Saunders / Elsevier; 2015.
- Hartman ME, Cheifetz IM. Pediatric Emergencies and Resuscitation. In: Kliegman RM, Stanton BF, St Geme JW, Schor NF, eds. Nelson Textbook of Pediatrics. 20th ed. Philadelphia, PA: Elsevier; 2016: Chapter 67.
- Horeczko T, Inaba AS. Cardiac Disorders. In: Walls RM, Hockberger RS, Gausche-Hill M, eds. Rosen’s Emergency Medicine: Concepts and Clinical Practice. 9th ed. Philadelphia, PA: Elsevier; 2018: Chapter 170.
- Navsaria PH, Nicol AJ, Edu S, Gandhi R, Ball CG. Selective nonoperative management in 1106 patients with abdominal gunshot wounds: conclusions on safety, efficacy, and the role of selective CT imaging in a prospective single-center study. Ann Surg. 2015;261(4):760-764.
- Olson K, Anderson I, Benowitz N, et al. Poisoning & Drug Overdose. 7th ed. Mc Graw-Hill Professional; 2018.
- Puskarich MA. Initial evaluation and management of abdominal gunshot wounds in adults. In: UpToDate. Editor: Moreira ME, Grayzel J; Mar 2015
- Saad Junior R, Carvalho WR de, Manoel XN, Forte V. Cirurgia Torácica Geral. 2˚ edição. Rio de Janeiro: Editora Atheneu; 2011.
- Sakles JC, Douglas MJK, Hypes CD, et al. Management of Patients with Predicted Difficult Airways in an Academic Emergency Department. J Emerg Med 2017; 53:163.
- Simons KJ, Simons FE. Epinephrine and its use in anaphylaxis: current issues. Curr Opin Allergy Clin Immunol 2010; 10:354.
- Skellett S, Hampshire S, Bingham R, Maconochie I, Mitchell S. European Paediatric Advanced Life Support. London: Resuscitation Council (UK); 2016.