Description
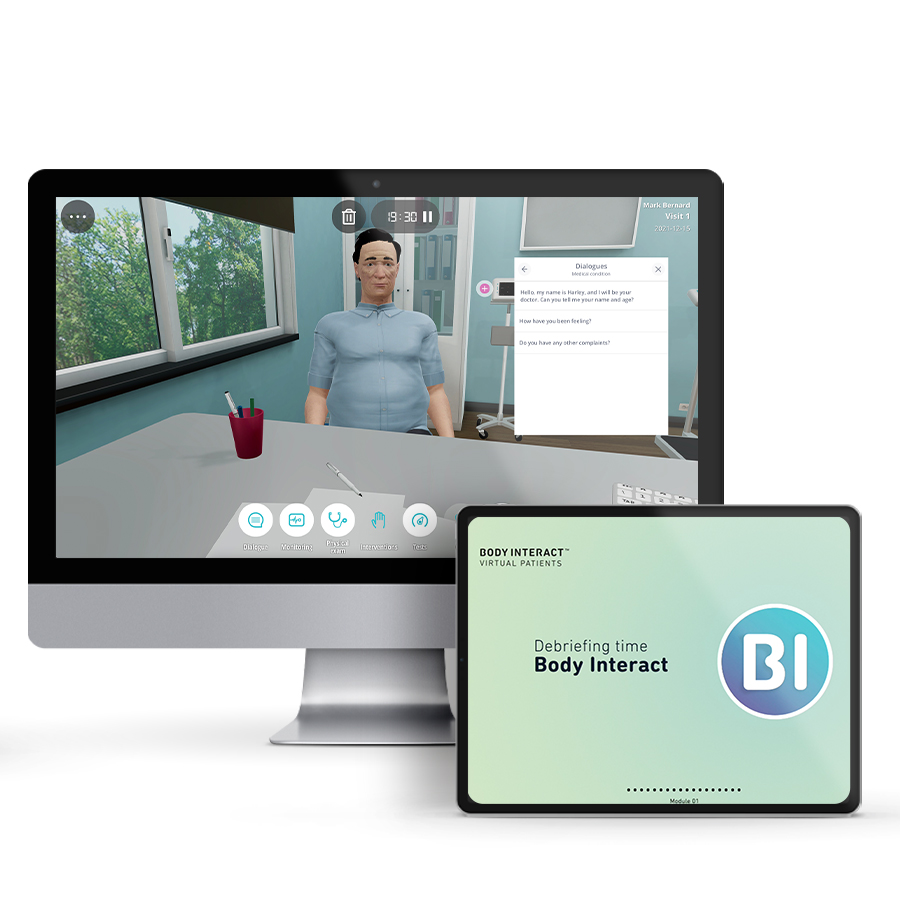
Course type: Online; Self-Paced
Specialty: Family Medicine
Language: English / Portuguese
Resources: Debriefing Videos
Level: Intermediate / Advanced
Target: Medical
Modules: 5
Durations: 2 months
Time Effort: Up to 110 minutes per module
Certificate: Yes
Course Description
Family medicine is defined as the medical specialty that manages common and long-term diseases in children and adults, focusing on overall health and wellness. The practice of family medicine physicians focuses on primary care settings such as chronic obstructive pulmonary diseases, diabetes, and others. This definition is based on the concept of common diseases, reflecting the reality that family physicians manage most health conditions in a community.
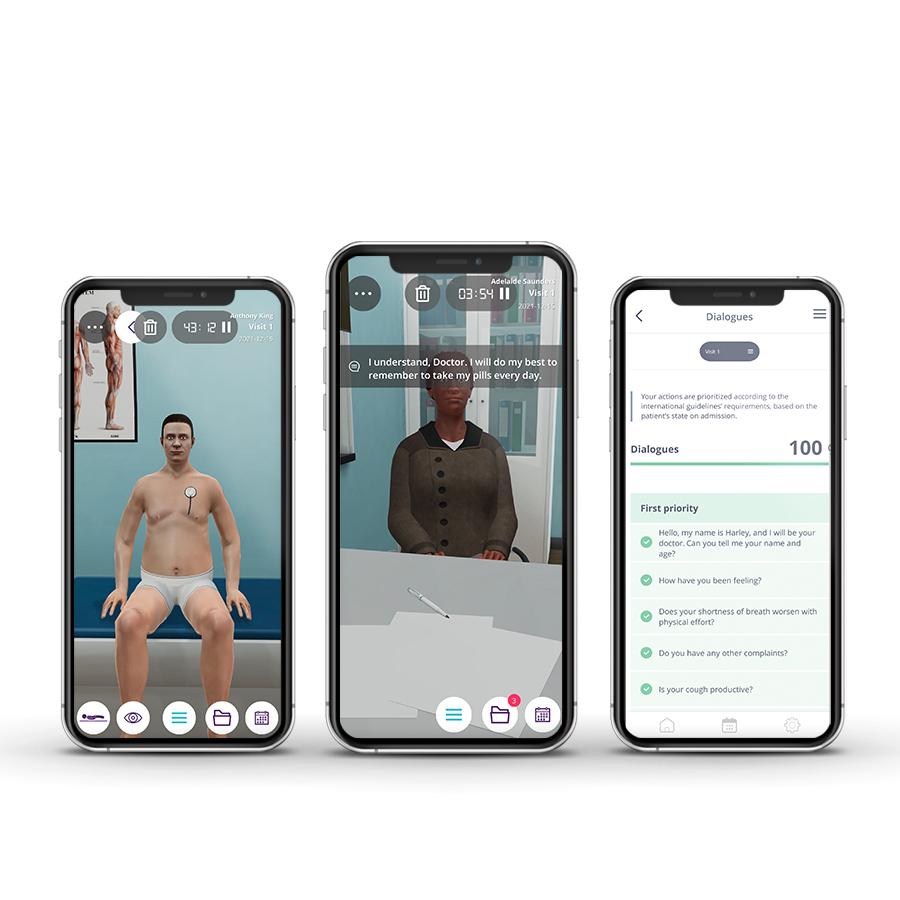
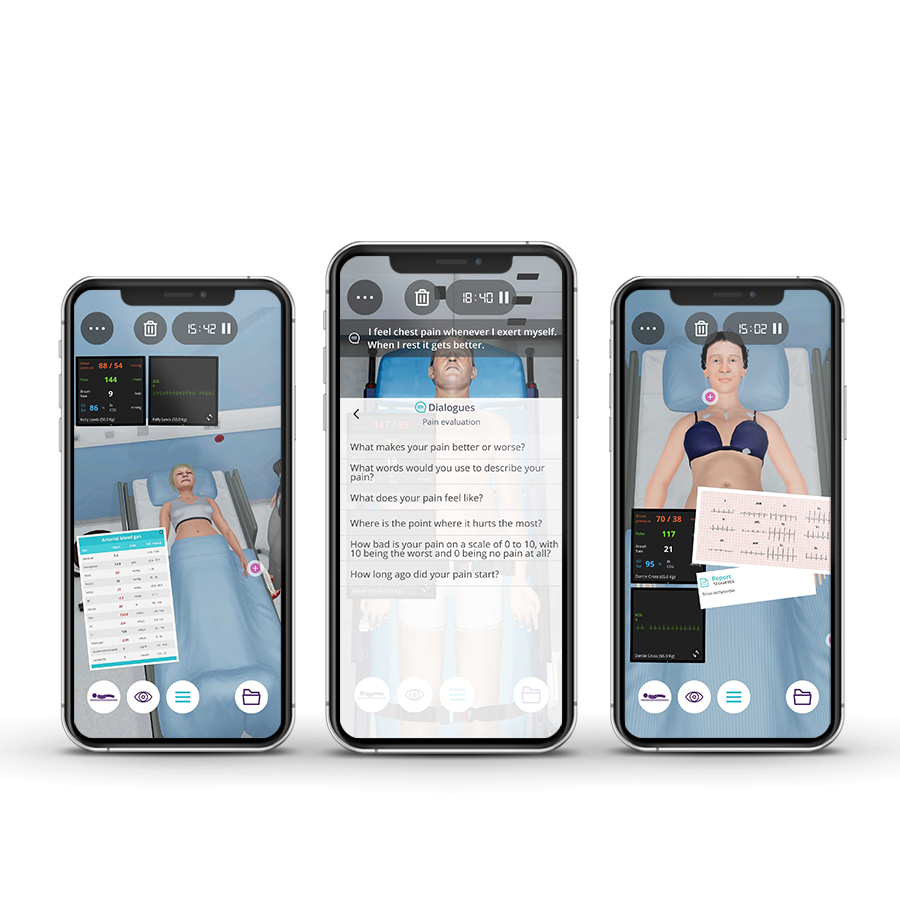
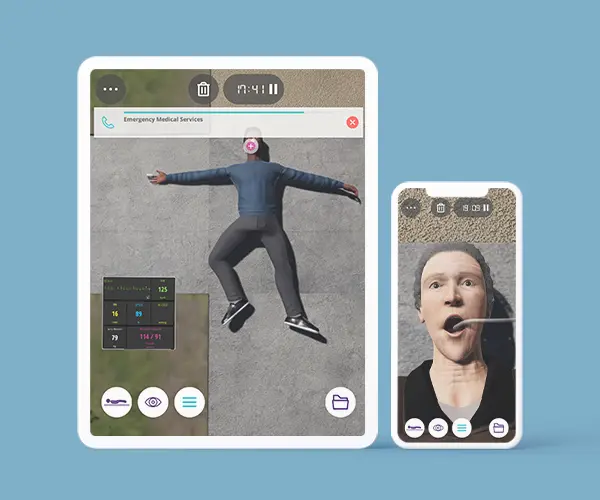
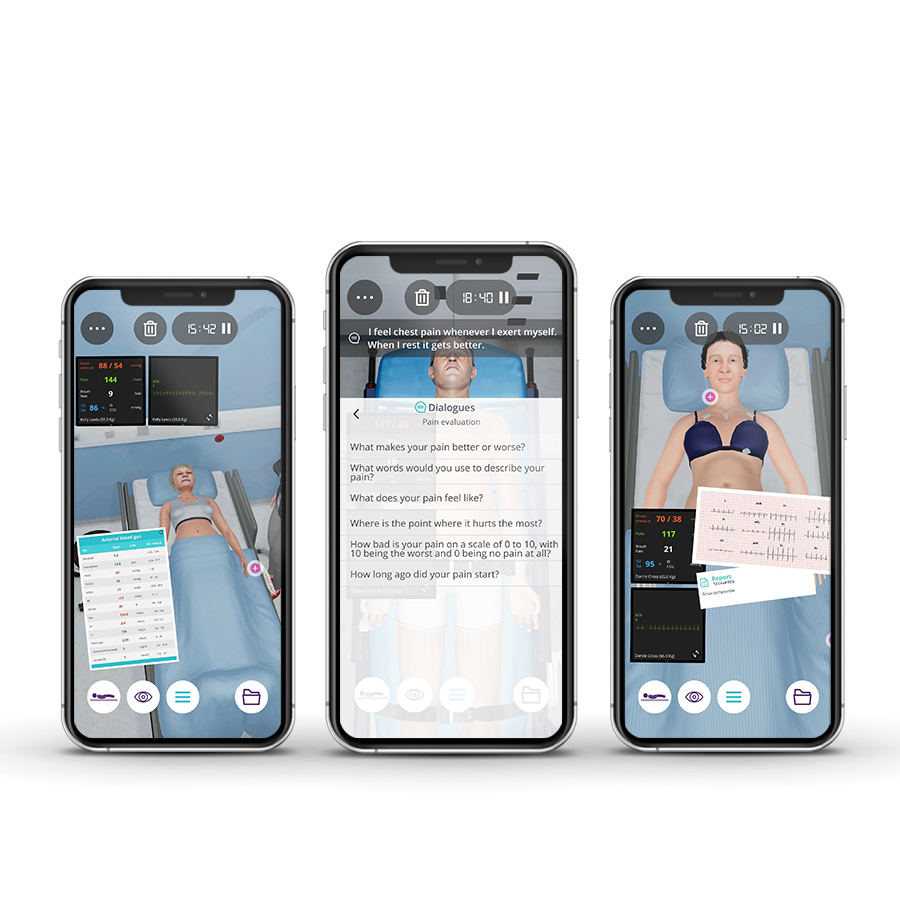
Family Medicine and General Practice course allow you, as a future resident, to develop your clinical reasoning and decision-making skills, practicing with a variety of adult patients in the medical appointment environment. Throughout this course, you will find five clinical scenarios of intermediate and advanced complexity in the allergology, respiratory, endocrinology, nephrology, and cardiology areas.
Course Overview
- 5 Modules
• The course consists of 5 modules, with each containing a Clinical Scenario. You can attempt each case up to 3 times. - Average Time to practice (per module)
• Clinical Scenario: 20 minutes per attempt (3 attempts: 60 minutes)
• Final attempt (if applicable): 20 minutes
• Multiple Choice Question: 5 minutes
• Feedback Area: 10 minutes
• Learning Objectives and Scientific References: 5 minutes
• Debriefing Video: 10 minutes - Online, Self-paced
• You have up to 2 months to complete the 10 modules at your own pace. The course can be accessed through Body Interact at any time. - Certificate of Completion
• After completing the course, you will receive a Certificate of Completion that can be added to your CV or Resume.
Learning Objectives
• Identify and control risk factors, namely obesity, and dyslipidemia;
• Diagnose chronic obstructive pulmonary disease (COPD) and identify possible risk factors;
• Diagnose type 2 diabetes (clinic and patient interrogation) and check fasting plasma glucose and glycated hemoglobin;
• Establish a therapeutic strategy plan (based on problems and evaluation strategy);
• Evaluate the efficacy of pharmacological and non-pharmacological prescriptions and the tolerance to pharmacological prescriptions;
• Evaluate vascular damage to target organs (retina/kidney/heart);
• Evaluate and management of Hereditary Angioedema (HAE) in the Outpatient Setting;
• Review treatment and weight control effect on glycemia;
• Manage chronic hyperkalemia in the outpatient setting;
• Treat coronary disease and manage multiple cardiovascular risk factors.
Clinical Competencies
Safety
• Universal safety measures procedures
• Promote patient safety
• Establish drug dosing for common medications
• Write prescriptions (including controlled drug)
Airway and Breathing
• Basic airway management
• Respiratory rate and rhythm assessment and interpretation
• Oximetry interpretation
• Basic spirometry (vital capacity, FEV 1 and interpretation)
• Thorax (shape, movement, diameter, ribs and diaphragm)
• Lung (percuss, fremitus, auscult and qualities of air sound, lobar locations) examination
Circulation
• Assess and interpret pulse (rate, rhythm and volume) and blood pressure
• Detect heart murmurs and identify S1 (tricuspid, mitral) and S2 (pulmonary, aortic) heart sounds and detect S3, S4 gallops
Disability
• Assess mental status (level of arousal, response to auditory stimuli, to visual stimuli, noxious stimuli)
• Cranial nerves assessment
• Blood sugar measurement and interpretation
Exposure
•Assess height and weight
• Lymph node assessment
• Cornea and anterior chamber assessment
• Gait and station and sensation assessment
• Skin test interpretation
• Motor function (voluntary movements, reflex withdraw, spontaneous, involuntary movements, tone)
• Interpretation of lab tests (Liver function, Renal function, Fluid/Electrolyte, Cardiac enzyme, Hematocrit, Arterial Blood Gas, coagulopathy rate interpretation, Lipid test, urinalysis, Thyroid test)
• Interpretation of imaging tests (Chest x-ray, Electrocardiogram interpretation, Ultrasonography, Nuclear imaging techniques, Computed tomography (CT) and Magnetic resonance imaging (MRI) result interpretation…)
• Abdominal examination (inspect, auscult, percuss and palp)
• Abdominal bruit
• Lens (clarity, artificial iol) and Disc (color, edges, size and shape) examination
• Ophthalmoscopic examination of fundi and retinae interpretation
• Nutrition management
Module 1 – Medical appointment for follow-up
Context: The presence of inherited conditions might be characterized by their recurrence. In this case, it has to be followed by family medicine physicians since the condition can be potentially fatal. The type, frequency, and severity of attacks vary between patients, and throughout the life of an individual patient.
Virtual Scenario: Anthony is being followed by an allergy/immunology outpatient clinic.
Module 2 – Referred for pulmonology appointment
Context: Lung disease can have diverse clinical presentations with multiple causes resulting in airflow limitation that is not completely reversible. Patients with these clinical conditions are at higher risk for the development of comorbidities and their surveillance is critical.
Virtual Scenario: Mr. Bernard felt unwell a few months ago, and his health was not improving. He visited his General Practitioner, who referred him to a visit Pulmonologist.
Module 3 – Unexplained weight loss
Context: Several symptoms presented by a patient may reveal clinical conditions that are critical to be evaluated by the family physician. Early detection reduces morbidity and mortality by preventing or delaying complications. A greater understanding of the clinical conditions underlying the presenting symptoms can result in more patient-specific and tailored management.
Virtual Scenario: Mr. Townsend has been relatively healthy his whole life. However, recently he started to notice unexplained weight loss and is thirsty most of the time.
Module 4 – Clinical status after angina episode
Context: The risk of progression or development of recurrent coronary artery disease after an acute episode is frequent and surveillance in the first few months is essential. Direct patient education is important and should be reinforced and documented.
Virtual Scenario: About a month ago, Adelaide required emergency medical care due to unstable angina. Today she has her first appointment for long-term health care management.
Module 5 – Easily fatigued with weakness and loss of appetite
Context: Fatigue is one of the most common complaints in medicine. Fatigue can be related to physical but also psychological symptoms. The anamnesis is very important to find out the meaning of the patient’s condition.
Virtual Scenario: Mr. Alexander has not been feeling well lately. In the past few months, his daily activities have been increasingly more difficult. Finally, his wife noticed he wasn’t well and persuaded him to visit his doctor.
Authors and Speakers
With a multidisciplinary group of international clinical reviewers, Body Interact ensures a high standard of accuracy, diversity, and impact of its course.
Paulo Martins
MD, PhD
Expert in Intensive Care
Faculty of Medicine, University of Coimbra, Portugal
Scientific References
- Agusti A, Beasley R, Celli BR, et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (2020 Report). Global Initiative for Chronic Obstructive Lung Disease; 2020.
- Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC Guideline for the Management of Patients With Non–ST-Elevation Acute Coronary SyndromesA Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64(24):e139-e228.
- Bakris GL, Pitt B, Weir MR, et al. Effect of Patiromer on Serum Potassium Level in Patients With Hyperkalemia and Diabetic Kidney Disease: The AMETHYST-DN Randomized Clinical Trial. JAMA. 2015;314(2):151-161.
- Bushinsky DA, Williams GH, Pitt B, et al. Patiromer induces rapid and sustained potassium lowering in patients with chronic kidney disease and hyperkalemia. Kidney Int. 2015;88(6):1427-1433.
- Craig T, Shapiro R, Vegh A, et al. Efficacy and safety of an intravenous C1-inhibitor concentrate for long-term prophylaxis in hereditary angioedema. Allergy Rhinol (Providence). 2017;8(1):e13-e19.
- Drawz PE, Babineau DC, Rahman M. Metabolic Complications are Common in Elderly Patients with Chronic Kidney Disease. J Am Geriatr Soc. 2012;60(2):310-315.
- Epstein M, Reaven NL, Funk SE, McGaughey KJ, Oestreicher N, Knispel J. Evaluation of the treatment gap between clinical guidelines and the utilization of renin-angiotensin-aldosterone system inhibitors. Am J Manag Care. 2015;21(11 Suppl):S212-220.
- FDA approves new drug to treat hyperkalemia. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm468546.htm. Accessed April 13, 2017.
- Food & Drug Administration (FDA). FDA Drug Safety Communication: FDA requires drug interaction studies with potassium-lowering drug Kayexalate (sodium polystyrene sulfonate). https://www.fda.gov/Drugs/DrugSafety/ucm468035.htm. Published October 22, 2015. Accessed April 13, 2017.
- Grundy Scott M., Stone Neil J., Bailey Alison L., et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol. Circulation. 0(0):CIR.0000000000000625.
- Healthcare Cost and Utilization Project (HCUP). https://www.ahrq.gov/research/data/hcup/index.html. Accessed April 12, 2017.
- Kovesdy CP. Management of Hyperkalemia: An Update for the Internist. The American Journal of Medicine. 2015;128(12):1281-1287.
- Latts LM, Reaven NL, Funk SE, McGaughey KJ, Adamson RT. Hyperkalemia Is Highly Prevalent In Patients With Cardiorenal Comorbidities Compared To Patients Without These Comorbidities. Value in Health. 2015;18(3):A135.
- Lepage L, Dufour A-C, Doiron J, et al. Randomized Clinical Trial of Sodium Polystyrene Sulfonate for the Treatment of Mild Hyperkalemia in CKD. CJASN. November 2015:CJN.03640415.
- Otani IM, Christiansen SC, Busse P, et al. Emergency Department Management of Hereditary Angioedema Attacks: Patient Perspectives. The Journal of Allergy and Clinical Immunology: In Practice. 2017;5(1):128-134.e4.
- Palmer BF, Clegg DJ. Hyperkalemia. JAMA. 2015;314(22):2405-2406.
- Reaven NL, Funk SE, Bakris GL. The economics of renoprotective therapy in advanced diabetic kidney disease. Am J Pharm Benefits. 2014;6(6):e169–e176.
- Relypsa Inc. Relypsa Submits Supplemental New Drug Application to FDA Requesting Label Changes for Veltassa Based on Phase 1 Drug-Drug Interaction Studies. GlobeNewswire News Room. http://globenewswire.com/news-release/2016/05/25/843419/0/en/Relypsa-Submits-Supplemental-New-Drug-Application-to-FDA-Requesting-Label-Changes-for-Veltassa-Based-on-Phase-1-Drug-Drug-Interaction-Studies.html. Published May 25, 2016. Accessed April 13, 2017.
- Rydén L, Grant PJ, Anker SD, et al. ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. European Heart Journal. 2013;34(39):3035-3087.
- Sterns RH, Grieff M, Bernstein PL. Treatment of hyperkalemia: something old, something new. Kidney International. 2016;89(3):546-554.
- Veltassa [Package Insert]. Redwood City, CA: Relypsa, Inc; 2016.
- Wedzicha JA, Calverley PMA, Albert RK, et al. Prevention of COPD exacerbations: a European Respiratory Society/American Thoracic Society guideline. European Respiratory Journal. 2017;50(3).
- Weir MR, Bakris GL, Bushinsky DA, et al. Patiromer in Patients with Kidney Disease and Hyperkalemia Receiving RAAS Inhibitors. New England Journal of Medicine. 2015;372(3):211-221.
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. January 2017:1-283.
- Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021-3104.