Description
Course type: Online; Self-Paced
Specialty: Specialty: Neurology
Language: English, Portuguese
Resources: Debriefing Videos
Level: Intermediate / Advanced
Target: Medical doctors
Modules: 14
Durations: 7 weeks
Time Effort: Up to 110 minutes per module
Certificate: Yes
Course Description
The occurrence of a cerebral event is extremely frequent, with ischaemic events being the most prevalent. The risk of stroke is closely linked to potentially identifiable risk factors such as high blood pressure, diabetes, atrial fibrillation, dyslipidemia, physical inactivity, smoking, and abdominal obesity. Although the benefits of a healthy lifestyle and the control of vascular risk factors are well documented, they remain poorly controlled.
Stroke is a medical emergency. The difference between recovery and death or disability depends on how effectively and quickly patients are treated. For healthcare professionals, it is imperative that an understand stroke and current evidence-based management. Treatment can dramatically improve the outcome of the patient.
The Masterclass In Cerebrovascular Emergencies Course (FMUL) is based on the European Stroke Organization Guidelines (2019, 2021) and the American Heart Association/American Stroke Association Guidelines (2019), so that professionals will improve their skills throughout the continuum of care in the emergency setting. This course allows for the development of clinical reasoning and clinical decision-making when faced with a stroke victim.
Course Overview
- 14 Modules
• 14 virtual patient cases of an intermediate level of complexity - 3 Webinars
• With medical experts from the Lisbon School of Medicine - Average Time to practice (per module):
• Clinical Scenario: 20 minutes per attempt (3 attempts: 60 minutes)
• Final attempt (if applicable): 20 minutes
• Multiple Choice Question: 5 minutes
• Feedback Area: 10 minutes
• Learning Objectives and Scientific References: 10 minutes
• Debriefing Video: 10 minutes - Online, Self-paced
• You have up to 7 weeks to complete the 14 modules at your own pace. The course can be accessed through Body Interact at any time. - Certificate of Completion
• Certified by Lisbon School of Medicine - 3 ECTS
Learning Objectives
• Recognize acute stroke and its subtypes
• Discuss the importance of early diagnosis of stroke
• Identify an ischemic stroke and search for its cause
• Perform neurological assessments using the “National Institute of Health Stroke Scale” (NIHSS) and detect neurological deficits
• Request the correct diagnostic tests to provide the most appropriate treatment
• Identify early ischemic lesions on brain CT and become familiar with the “Alberta stroke program early CT score” (ASPECTS)
• Identify a large vessel occlusion on CT angiography
• Participate in reperfusion therapy decision: intravenous thrombolysis (alteplase), endovascular therapy (thrombectomy), both or none
• Be familiar with relative and absolute contraindications to alteplase
• Discuss indication for thrombectomy with interventional neuroradiology
• Manage blood pressure in acute ischemic or hemorrhagic stroke
• Manage patients with acute ischemic or hemorrhagic stroke while taking oral anticoagulants
• Discuss prognosis and how to transmit bad news to the family members
• Manage patients with minor stroke or transient ischemic attack
• Discuss antithrombotic decisions in secondary stroke prevention
• Discuss etiology and treatment options for hemorrhagic stroke
Module 1 – Right side weakness
Context: A greater proportion of patients with no-to-minimal pre-stroke disability achieve an excellent functional outcome if they receive appropriate treatment in a timely manner. International guidelines currently recommend intravenous thrombolysis (alteplase) for patients with ischemic stroke with less than 4h30 since symptoms onset, provided there are no contra-indications.
Virtual Scenario: Mr. Howarth lying on the floor of his house with right-sided weakness, including facial asymmetry, when he was found by his wife. He had been seen well two hours before. The wife immediately called the emergency unit, and he was brought to the hospital.
Module 2 – Sudden right-sided weakness and abnormal speech
Context: The existence of signs and symptoms can lead to a clinical diagnosis of stroke, for which there are treatments that can improve the prognosis. However, there are conditions where therapeutic interventions are not helpful or effective, and in some cases, they can be harmful.
Virtual Scenario: Mr. Antonio was at home with his wife, when he began to feel difficulty in speaking and weakness. His wife called the paramedics, which quickly transported Mr. Antonio to the emergency room.
Module 3 – Found collapsed in his living room
Context: International guidelines currently recommend endovascular treatment (thrombectomy) in case of acute ischemic stroke due to intracranial large vessel occlusion, in patients with less than 6 hours from the onset and without pre-stroke disability.
Virtual Scenario: Mr. Williamson lying on the floor of his house with left-sided weakness, including facial asymmetry, when he was found by his daughter. The daughter immediately called the emergency unit, and he was brought to the hospital.
Module 4 – Sudden weakness on right side and impaired speech
Context: Increased sympathetic tone causes hypertension after a cerebral event, and blood pressure management in acute stroke is fundamental, particularly when reperfusion therapy is required.
Virtual Scenario: When taking care of her grandchildren, Mrs. Smith suddenly experienced difficulty in moving her right arm. Her family also noticed that she had facial asymmetry and was not talking properly.
Module 5 – Acute stroke with arrhythmia
Context: The size and location of the stroke may correlate with the severity and type of symptoms. The location of vascular occlusion should be taken into account when deciding on revascularization therapy. A careful clinical history should be taken to support the decision about the reperfusion therapy for each patient.
Virtual Scenario: While having dinner at home, Mr. Fox suddenly experienced difficulty in talking and moving his right arm. His wife called for 112 as soon as she could.
Module 6 – Collapsed after getting up from bed
Context: Many patients have a stroke while they are sleeping, so the time of onset cannot be determined. This raises a dilemma about brain tissue viability and the benefit of revascularization therapy.
Virtual Scenario: Mr. Stevenson collapsed after trying to get up from bed at 8 am. His wife noticed that he could not move his left body and called 112. He had gone to bed at 10 pm and spoke with his wife at the time.
Module 7 – Aphasia and lack of strength in the right arm with unknown onset time
Context: Some stroke symptoms, such as aphasia or anosognosia, may prevent the patient from explaining the time of onset, which is essential information to be a candidate for revascularization therapies. In such cases, it is necessary to draw on all information from family members or use advanced brain imaging tests.
Virtual Scenario: Mrs. Joplin was found at home slumped on the floor by her daughter. When asked about the last time she had seen her mother well, the daughter mentioned that it was about 12/13 hours ago.
Module 8 – Brain death
Context: Declaration of brain death requires demonstration of irreversible injury to the whole brain including the brainstem. Current guidelines rely on bedside clinical examination to determine that the patient has irreversible coma, absent brainstem reflexes, and apnea.
Virtual Scenario: While with his family, the patient suddenly displayed signs of severe illness: he could not move his right side and started vomiting.
Module 9 – Sudden focal symptoms in a patient on anticoagulation
Context: Patients with atrial fibrillation and under anticoagulation are at risk of having an ischemic or hemorrhagic stroke. The management of these patients, when they appear with focal signs, is complex and it is necessary to decide which treatment is indicated.
Virtual Scenario: Ms. Parrish suddenly felt right-sided weakness and couldn’t express herself while she was having a meal. Her son noticed her face was dropping to the side and immediately called the emergency unit.
Module 10 – I’m much better now
Context: Patients with symptoms strongly suspected of having a stroke should be transported rapidly the hospital irrespective of the intensity of the symptoms to quickly assessment and adequately treatment. Close monitoring is needed even for those who improve.
Virtual Scenario: Ms. Santos was at home with her daughter, when she began to feel difficulty in speaking and weakness. Her daughter called the paramedics, who transported Ms. Santos to the emergency room. When she arrived, the symptoms had markedly improved.
Module 11 – Now I’m fine
Context: Focal brain or retinal deficits may be transient and resolved within 24h, and are known as transient ischemic attacks (TIA). International guidelines currently recommend urgent evaluation for patients with a TIA, to prevent recurrent vascular events
Virtual Scenario: While watching TV, Mrs. Silva complained to her daughter of a lack of strength in her left arm and leg. She promptly was taken to the hospital but recovered fully until arriving there.
Module 12 – Sudden headache and right side weakness
Context: Spontaneous intracerebral hemorrhage has higher mortality and morbidity than ischemic stroke, and it is essential to recognize its cause. Excellent medical care may have a strong potential impact on prognosis.
Virtual Scenario: Mr. Mendes was leaving the car park with his son when he started complaining of a headache and fell. His son saw that he was not well and immediately called the medical emergency number (112).
Module 14 – Slurred speech and motor impairment in the left arm in a patient taking warfarin
Context: The occurrence of focal signs in a patient with atrial fibrillation treated with anticoagulant should lead to the differential diagnosis of different brain lesions. In case they are caused by intracerebral hemorrhage, the patient must be treated properly to avoid a poor prognosis.
Virtual Scenario: Mrs. Amelia was with her grandson at home doing lunch when suddenly she started with slurred speech, facial asymmetry, and difficulty in moving her left arm.
Module 13 – Sudden weakness on left side
Context: A cerebral event leads to serious sequelae for the patient if not addressed in a timely manner. It is essential to discuss acute treatment in patients with associated pathologies and under specific therapies, such as anticoagulation.
Virtual Scenario: Mr. Pearson suddenly felt weakness in his left arm and leg. His family quickly called for an ambulance to take him to a Central Hospital.
Authors and Speakers
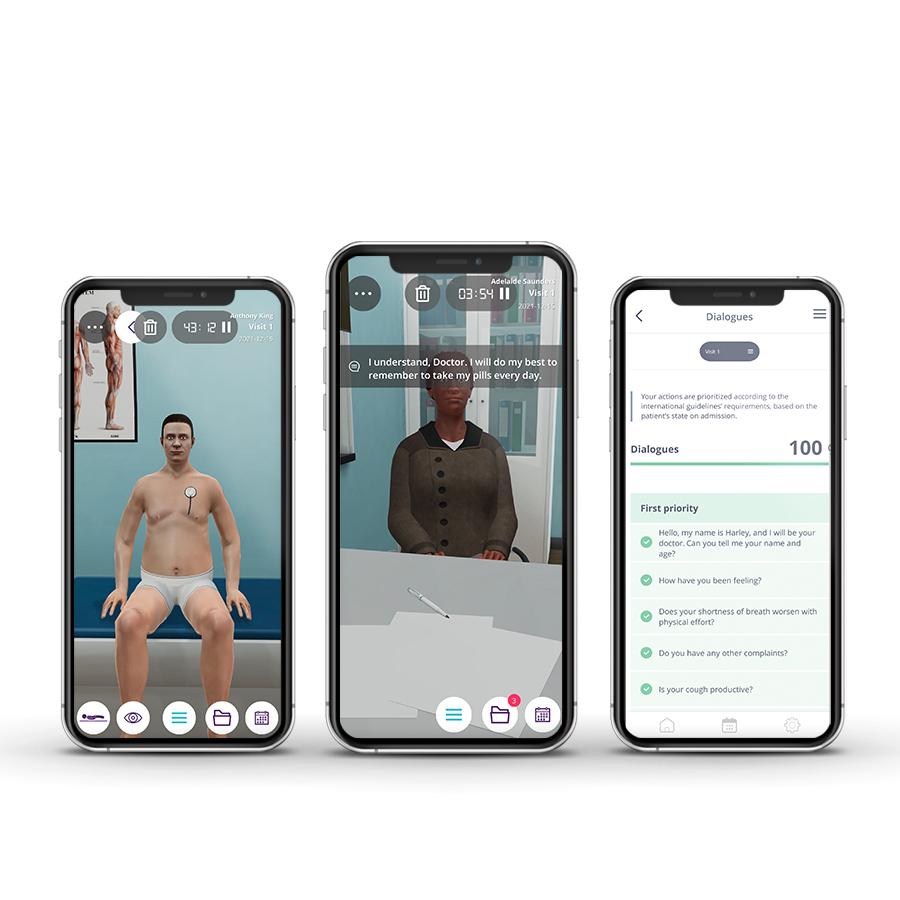
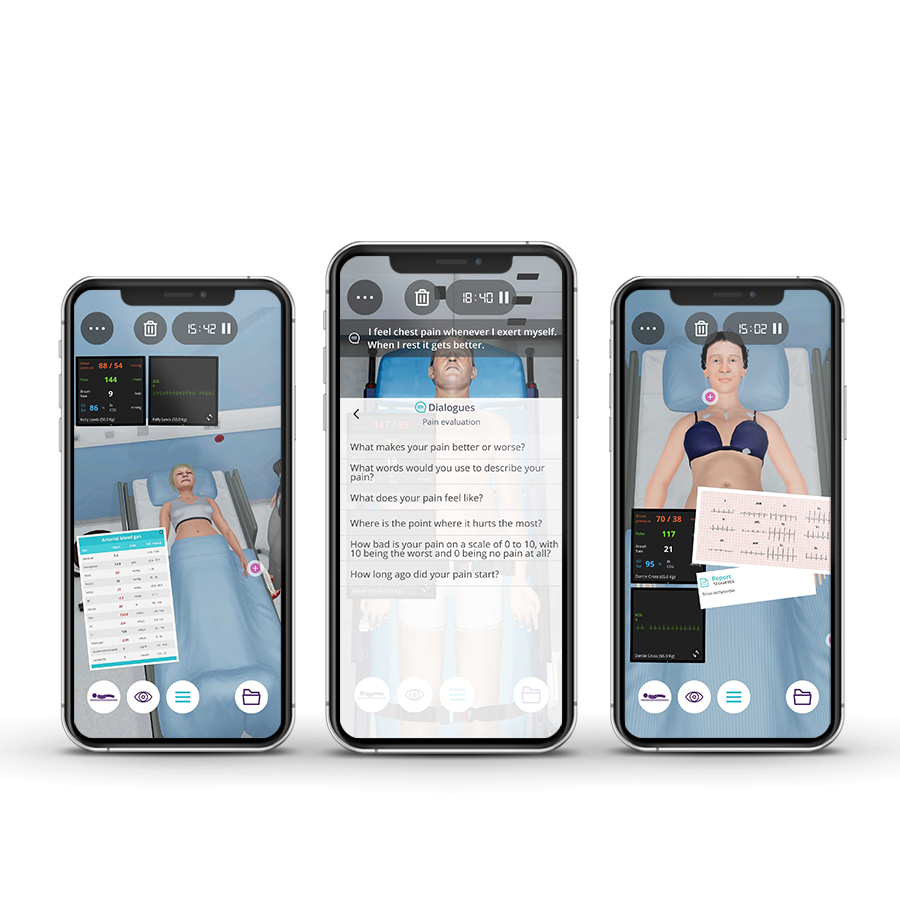
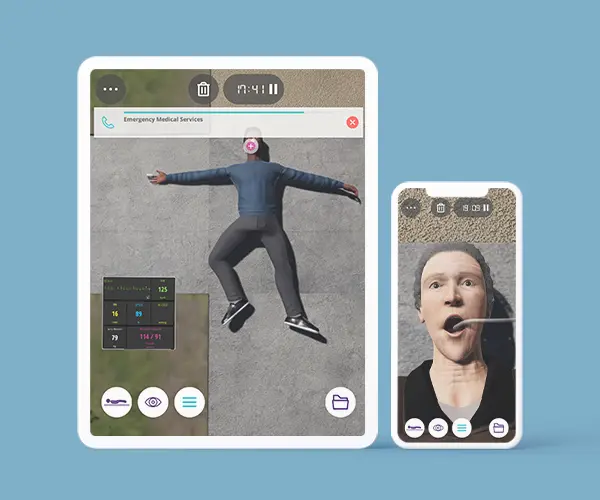
With a multidisciplinary group of international clinical reviewers, Body Interact ensures a high standard of accuracy, diversity, and impact of its course.
Course Coordinator
Patrícia Canhão
MD, PhD
Stroke Unit, Hospital de Santa Maria|Lisbon School of Medicine of Lisbon
Lia Lucas Neto
MD, PhD
University of Lisbon | UL · Faculty of Medicine
Catarina Fonseca
MD, PhD
Stroke Unit, Hospital de Santa Maria | Lisbon School of Medicine of Lisbon
Pedro Alves
MD, PhD
Stroke Unit, Hospital de Santa Maria | Lisbon School of Medicine of Lisbon
Mariana Dias
MD
Stroke Unit, Hospital de Santa Maria | Lisbon School of Medicine of Lisbon
Scientific References
- Albers, GW, Marks, MP, Kemp, S, et al; DEFUSE 3 Investigators. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018;378:708–718.
- Berge E, Whiteley W, Audebert H, et al. European Stroke Organisation (ESO) guidelines on intravenous thrombolysis for acute ischaemic stroke. European Stroke Journal. 2021;6(1):I-LXII.
- Campbell BCV, Hill MD, Rubiera M, et al. Safety and Efficacy of Solitaire Stent Thrombectomy: Individual Patient Data Meta-Analysis of Randomized Trials. Stroke. 2016;47(3):798-806.
- Emberson J, Lees KR, Lyden P, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet. 2014;384(9958):1929-1935.
- Fonseca, A. C., et al. (2021). European Stroke Organisation (ESO) guidelines on management of transient ischaemic attack. European Stroke Journal, 2396987321992905.
- Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387(10029):1723-1731.
- Greer DM. Determination of Brain Death. N Engl J Med. 2021;385(27):2554-2561
- Hemphill JC 3rd et al. Guidelines for the Management of Spontaneous Intracerebral Hemorrhage. A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2015 Jul;46(7):2032-60.
- Kernan, W. N., et al. (2014). Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, 45(7), 2160-2236.
- Kleindorfer D, et al. 2021 Guideline for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack: A Guideline From the American Heart Association/American Stroke Association. AHA journals. 2021;7 (52).
- Lemmens R, Hamilton SA, Liebeskind DS, et al. Effect of endovascular reperfusion in relation to site of arterial occlusion. Neurology. 2016;86(8):762-770.
- Nogueira, RG, Jadhav, AP, Haussen, DC, et al. DAWN Trial Investigators. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018;378:11–21.
- Pexman JH, Barber PA, Hill MD, et al. Use of the Alberta Stroke Program Early CT Score (ASPECTS) for assessing CT scans in patients with acute stroke. AJNR Am J Neuroradiol. 2001;22(8):1534-1542.
- Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344-e418.
- Sandset EC, Anderson CS, Bath PM, et al. European Stroke Organisation (ESO) guidelines on blood pressure management in acute ischaemic stroke and intracerebral haemorrhage. European Stroke Journal. 2021;6(2):XLVIII-LXXXIX.
- Shemie SD, Hornby L, Baker A, et al. International guideline development for the determination of death. Intensive Care Med. 2014;40(6):788-797.
- Steiner T, Al-Shahi Salman R, Beer R, et al. European Stroke Organisation (ESO) guidelines for the management of spontaneous intracerebral hemorrhage. Int J Stroke. 2014;9(7):840-855.
- Thomalla G, Boutitie F, Ma H, et al. Intravenous alteplase for stroke with unknown time of onset guided by advanced imaging: systematic review and meta-analysis of individual patient data. Lancet. 2020;396(10262):1574-1584.
- Thomalla G, Simonsen CZ, Boutitie F, et al. MRI-Guided Thrombolysis for Stroke with Unknown Time of Onset. New England Journal of Medicine. 2018;379(7):611-622.
- Turc G, Bhogal P, Fischer U, et al. European Stroke Organisation (ESO) – European Society for Minimally Invasive Neurological Therapy (ESMINT) Guidelines on Mechanical Thrombectomy in Acute Ischaemic StrokeEndorsed by Stroke Alliance for Europe (SAFE). European Stroke Journal. 2019;4(1):6-12.
- Van der Worp, H. B., Hofmeijer, J., Jüttler, E., Lal, A., Michel, P., Santalucia, P.,& Thomalla, G. European Stroke Organisation (ESO) guidelines on the management of space-occupying brain infarction. European Stroke Journal, 2021.
- Wardlaw JM, Murray V, Berge E, del Zoppo GJ. Thrombolysis for acute ischaemic stroke. Cochrane Database Syst Rev. 2014;(7):CD000213.